The Concept of Movement Literacy for Joint Replacement Fitness Clients
In 2009, 438,000 hip and 686,000 knee arthroplasties were performed in the United States, but a 2019 study projected the numbers for 2025 and 2030 to be…
Lost your password? Please enter your email address. You will receive a link to create a new password.

In 2009, 438,000 hip and 686,000 knee arthroplasties were performed in the United States, but a 2019 study projected the numbers for 2025 and 2030 to be…
“We have a brain for one reason and one reason only, and that’s to produce adaptable and complex movements.” This quote may come as a surprise. As we are often only concerned with our client’s muscles, joint, lungs, and hearts. The reality is that all training is brain training, we just don’t think of it that way.
In Part 1 of this article, we defined isometrics and discussed the two basic types of isometric exercises, yielding and overcoming, and why you might choose one over the other. In Part 2, we’re going to discuss the benefits of isometrics, especially for joint replacement clients, and ideas on how to use and program isometrics.
Isometric exercises are beneficial for everyone – athletes, fitness enthusiasts, those with musculoskeletal pain, those in rehab, etc. But they are especially beneficial for joint replacement fitness. Here are the primary benefits of isometrics training:
You control the effort level – The client has complete control over the amount of effort/force they are producing. This not only contributes to the safety of isometric training, but it also helps joint replacement clients (or anyone recovering from injury or motor control issues) learn how to control their force production. Isometrics specifically activate pre-motor and supplementary motor areas in the brain.
Isometrics are the least neurologically threatening form of strength training[1] – Because the client is in total control of the effort level and that force is being produced without joint movement, isometrics are a very low threat to the nervous system. This very often allows clients to utilize isometrics well before dynamic exercises, and feel safe producing force, which is very important as joint replacement clients relearn neuromuscular activation patterns.
Larger amounts of force can be generated than dynamic training – If you are doing multiple reps of an exercise, you are, by definition, not producing maximum force. Isometrics allow a client to work up to max force production in a safe and pain-free manner.
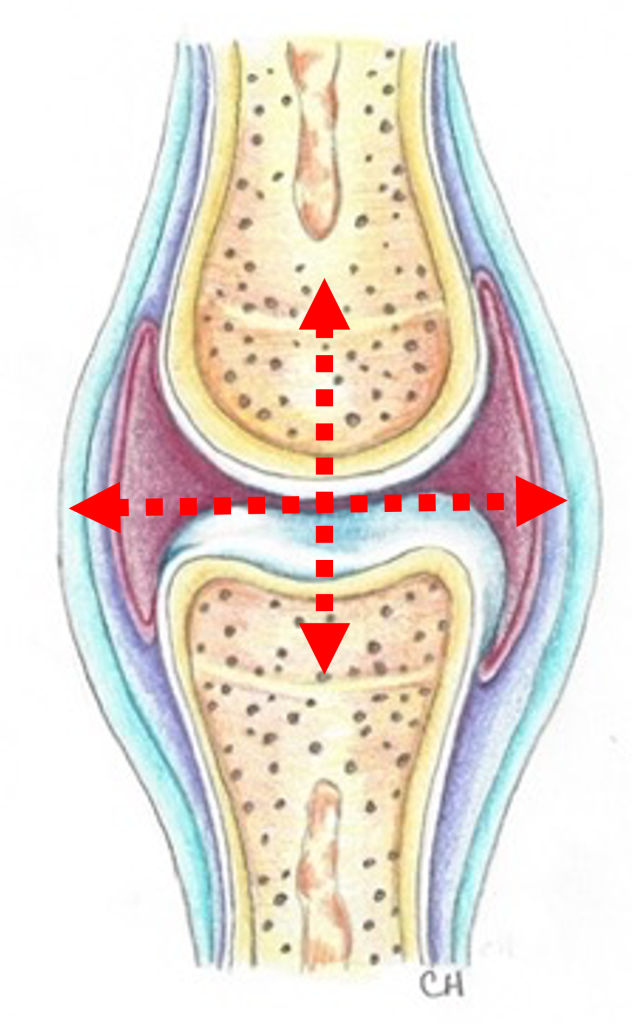
Isometrics promote joint health and strength – The synovial fluid in joints is a Non-Newtonian Fluid, meaning that when increased pressure occurs through the joint, the viscosity of the synovial fluid increases, to provide more protection for the joint. Thus, isometrics take advantage of the hydrodynamics of the joint fluid, which increases joint stability as increasing amounts of force are put through the joint.
Pain reduction – Isometric exercises have been shown to reduce pain in patellar tendinopathy[1] and lateral elbow tendinopathy[2], sometimes used by itself or with other modalities. In our experience, isometrics can be a very powerful tool to mitigate musculoskeletal pain.
There are three primary parameters we can adjust when doing isometrics:
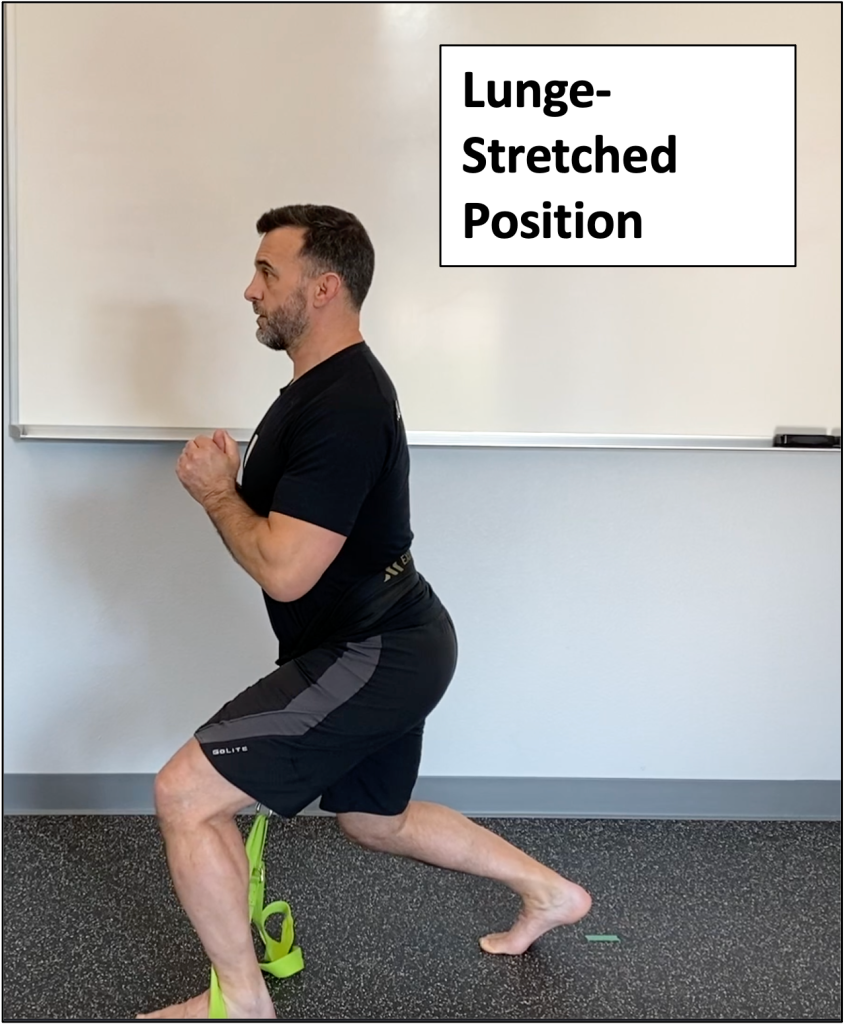
A good place to start with joint replacement clients would be lower effort levels, longer times of contraction, and the most comfortable joint angle. For a knee replacement client this could look something like:


Unilateral, open chain exercises like these are great as they force stabilization to happen on the non-working side, so you would want the client to do isometrics on both sides. When the non-replaced side is doing the isometric, the replacement side must do the stabilization. This is just as important as the strength work. However, depending on the client’s starting point for stabilization, you may need to start with closed chain exercises.
As the joint replacement client becomes stronger and more stable, you could shift into higher effort levels, shorter times of contraction, and multiple joint angles. For a hip replacement client this could look something like:
Isometrics can be a very useful and powerful tool when training joint replacement clients but also for general fitness, performance, and pain clients! You can learn more about isometrics, specific isometric exercises for joint replacement clients, and about taking a neuro-centric approach to medical fitness with our Joint Replacement Fitness Specialist online course, available through the MedFit Classroom!

Pat Marques is a Z-Health Master Trainer and NSCA-CPT specializing in training the nervous system to improve performance and get out of pain. After retiring from the Active Duty Army, Pat pursued his education and certifications in exercise science, initially working with wounded, ill, and injured soldiers. During this time that Pat discovered the power of using a neurological approach to training to get out of pain and improve fitness and performance. He currently provides exercise therapy, movement reeducation, and strength and conditioning for all levels of clients at NeuroAthlete, from chronic pain sufferers to Olympic-level and professional athletes.
References
[1] Cobb, E. (2017). 9S: Strength & Suppleness Course, Z-Health Performance Solutions.
[2] van Ark M, et al. (2015). Do isometric and isotonic exercise programs reduce pain in athletes with patellar tendinopathy in-season? A randomised clinical trial. J Sci Med Sport (2015).
[3] Vuvan, V., Vicenzino, B., Mellor, R., Heales, L., & Coombes, B. (2019). Unsupervised Isometric Exercise versus Wait-and-See for Lateral Elbow Tendinopathy. Medicine & Science in Sports & Exercise.
[4] Kubo, K., Ohgo, K., Takeishi, R., Yoshinaga, K., Tsunoda, N., Kanehisa, H., & Fukunaga, T. (2005). Effects of Isometric training at different knee angles on the muscle-tendon complex in vivo. Scandinavian Journal of Medicine & Science in Sports.

Isometric exercises are the most highly under-utilized form of exercise in fitness in general, but they are especially important in a medical fitness context. In this two-part blog series we’re going to discuss what isometrics are, why they are so good (especially for joint replacement fitness), and how you can use them.
In Part 1, let’s define what we are talking about.

Isometric exercises utilize an isometric contraction of the muscle, which is a contraction in which the muscle is neither shortening nor lengthening as the muscle contracts. A concentric contraction is when the muscle belly is shortening as the muscle contracts (e.g., flexing the elbow as you raise the weight during a biceps curl). An eccentric contraction is when the muscle belly is lengthening as the muscle contracts (e.g., extending the elbow as you lower the weight during a biceps curl).
With isometrics we are contracting/flexing the muscle, but there is no movement (shortening or lengthening) of the muscle.
There are many ways to do isometrics, but they all essentially fall into two broad categories:
Yielding isometrics
Yielding isometrics are when you are trying to resist a force, weight, or gravity. These are sometimes called “holding” isometrics. If you were a disruptive student in gym class as a kid, like me, you may fondly remember wall sits… a great example of a yielding isometric exercise.
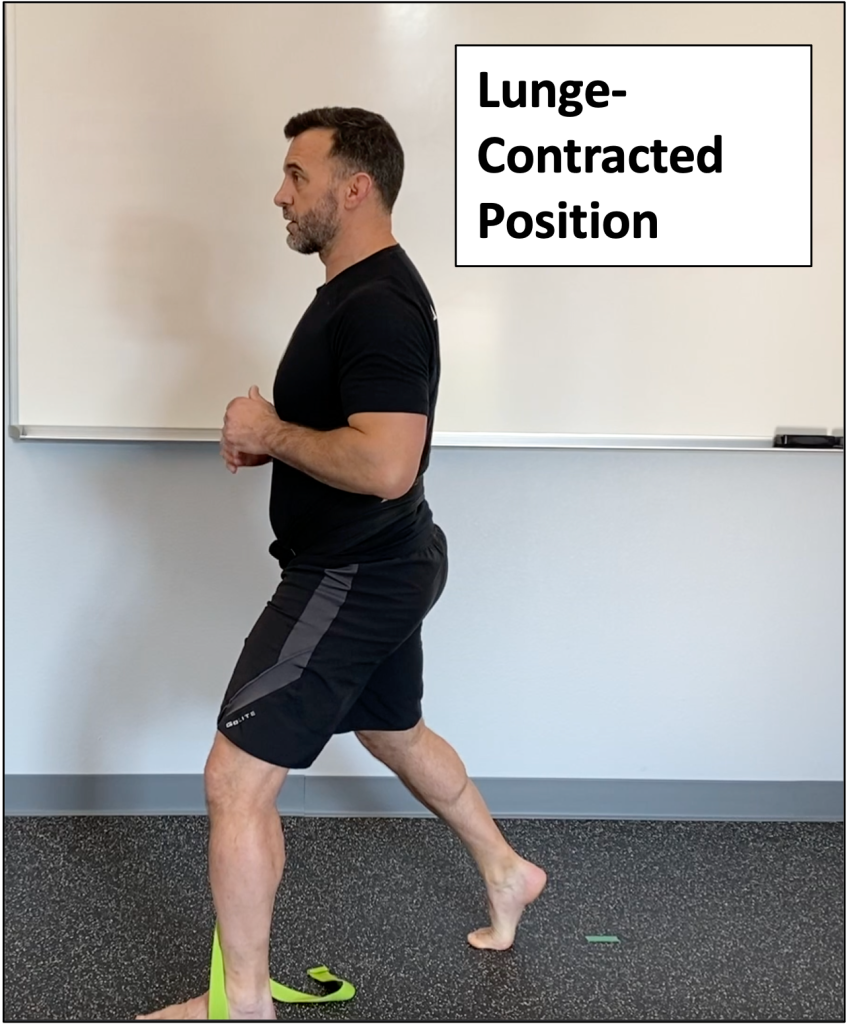
With yielding isometrics, think deceleration. You are essentially fighting the eccentric (lengthening) contraction. Other examples include:
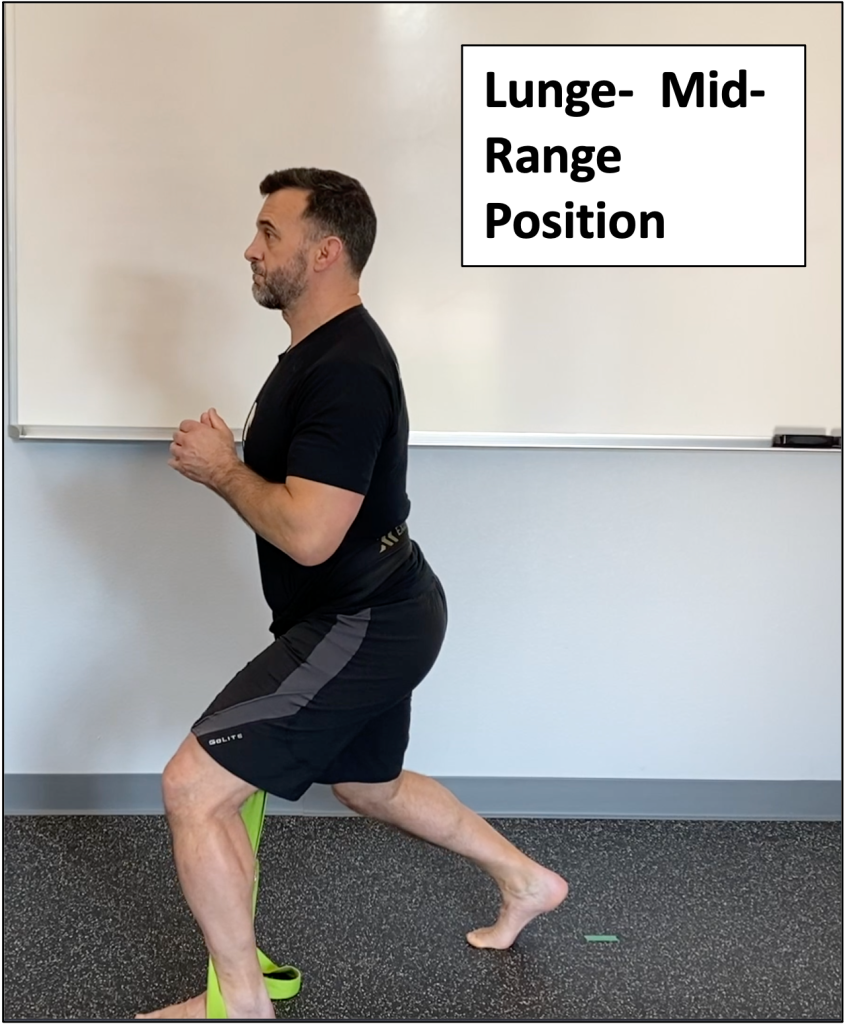
You do not have to be in the fully contracted position like the two examples above. Holding a mid-range position, like the wall sits example or holding a weight halfway through a rep range, would also be a yielding isometric.

Overcoming isometrics
Overcoming isometrics are when you are trying to produce force against an object that will not move. These are sometimes called “pushing” isometrics.
With overcoming isometrics, think acceleration. You are engaging the concentric (shortening) contraction, but the shortening of the muscle is blocked by the immovable object (i.e., bar, strap, etc.). Using a hip belt connected to a strap you are standing on would be an example for a squat pattern. Other examples include:

Both types of isometrics are very useful for regaining muscular force production capability. Some studies have shown that under equal force generation, a muscle will fatigue faster during a yielding isometric, possibly due to the more complex neural control strategies involved.[1]
When choosing between the two types, consider the SAID Principle – Specific Adaptation to Imposed Demand. Does your joint replacement client most need to work on getting up out of a chair? If so, then overcoming isometrics will likely help them the most (more concentric contraction focused). Conversely, if they are having the most difficulty in descending stairs, yielding isometrics may be of more benefit (more eccentric contraction focused).
In Part 2, we’ll talk about the specific benefits of isometrics, especially for joint replacement clients, and ideas on how to use and program isometrics.
Begin learning a neuro-centric approach to medical fitness and how to work with joint replacement clients with our Joint Replacement Fitness Specialist online course, available through the MedFit Classroom!

Pat Marques is a Z-Health Master Trainer and NSCA-CPT specializing in training the nervous system to improve performance and get out of pain. After retiring from the Active Duty Army, Pat pursued his education and certifications in exercise science, initially working with wounded, ill, and injured soldiers. During this time that Pat discovered the power of using a neurological approach to training to get out of pain and improve fitness and performance. He currently provides exercise therapy, movement reeducation, and strength and conditioning for all levels of clients at NeuroAthlete, from chronic pain sufferers to Olympic-level and professional athletes.
References:
[1] Schaefer, L & Bittmann, F. (2017). Are there two forms of isometric muscle action? Results of the experimental study support a distinction between a holding and a pushing isometric muscle function. BMC Sports Science, Medicine, and Rehabilitation, 9:11.

Proprioception refers to the conscious and unconscious perception of postural balance, muscles sense, and joint position and stability. Basically, it is your sense of where you are in time and space for movement. We have found over the years that the best way to explain proprioception to clients comes from Dr. Eric Cobb at Z-Health Performance Solutions:
“Proprioception is the body’s 3D map of itself in time and space. AKA our movement and awareness map”.
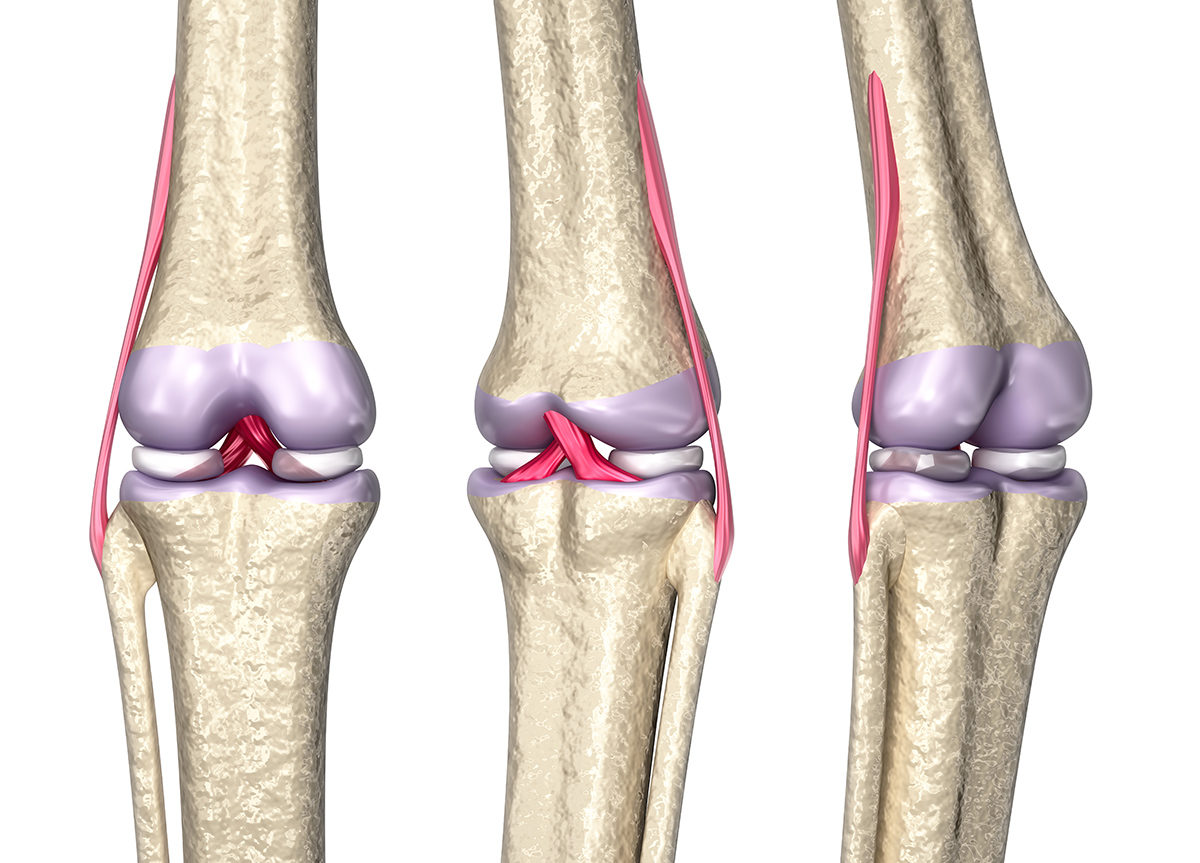
The detail and definition of this “proprioceptive map” comes from several specialized mechanoreceptors (i.e. nerve endings) in the muscles, tendons, joint capsules, fascia, and skin. As fitness trainers as we are usually taught about muscle spindles and Golgi tendon organs when we learn about flexibility training, but there is a lot more to proprioceptive input. You are affecting the proprioceptive input to the brain when you use a neoprene knee sleeve (pressure), kinesiology tape (skin stretch), heat or ice packs (temperature), TENS units (electric), etc.
Several conditions can alter proprioception, thus “clouding” the map and degrading movement sense and capability, including pain, trauma, effusion, and fatigue. A joint replacement client also likely had poor motor control of the joint in the first place that resulted in compensatory movement patterns and overuse injury over time. Complicating the matter further, although it may have been necessary, the surgery itself is an “insult” to the musculoskeletal and nervous systems.

To move a joint well, you must be able to feel the joint and surrounding tissue well. An extreme example of what can happen without the sense of touch or joint position is the story of Ian Waterman. A rare neurological illness resulted in his losing all touch and joint position sensation, effectively paralyzing him from the neck down even though the motor control area of his brain and the descending pathways to send movement information to his musculature were fine!
We can improve proprioception in several ways:
The important take away is that building a “library” of prior movement patterns is especially important for the post-medical joint replacement client. We want to get their new joint moving in multiple directions, at multiple speeds, under multiple loads.
The concept of proprioception and how to harness it is not only for joint replacement, but also for general fitness, performance, and pain clients! Begin learning a neuro-centric approach to medical fitness and how to work with joint replacement clients with our Joint Replacement Fitness Specialist online course, available through the MedFit Classroom!
Pat Marques is a Z-Health Master Trainer and NSCA-CPT specializing in training the nervous system to improve performance and get out of pain. After retiring from the Active Duty Army, Pat pursued his education and certifications in exercise science, initially working with wounded, ill, and injured soldiers. During this time that Pat discovered the power of using a neurological approach to training to get out of pain and improve fitness and performance. He currently provides exercise therapy, movement reeducation, and strength and conditioning for all levels of clients at NeuroAthlete, from chronic pain sufferers to Olympic-level and professional athletes.
References:

The SAID Principle, Specific Adaptation to Imposed Demand, is a fundamental law of human physiology. The classic definition of this principle is “the body adapts to what it does”. A more precise, neuro-centric definition would be “the body ALWAYS adapts to EXACTLY what it does”. The takeaway is this: if you want a certain result, you must train with precision.

Joint replacements are an incredible medical innovation, but they are also incredibly traumatic events to the dermal, fascial, musculoskeletal, and nervous systems. Of specific concern for joint replacement clients are the mechanoreceptors that provide input to the brain about the joint and surrounding area through touch, pressure, stretch (skin and muscles/tendons), temperature, vibration, and movement.
Some studies have shown, depending on the type of replacement performed, joint capsule mechanoreceptors are no longer present and do not regenerate. The injuries to tissues or joints, whether acute or chronic, can result in dysfunctional proprioceptive feedback, and that is not automatically regained after joint replacement. So, we will need to train with precision to maximize and improve proprioceptive input and joint position sense.
Training with precision means taking our fitness training beyond “strengthening and stretching”. Our joint replacement clients likely got plenty of that during their physical therapy anyway. Another way to think about the SAID Principle is “use it or lose it”. If we want our joint replacement fitness clients to get the most out of their replacement, we need to program a variety of aspects:
Programming for this type of variety is very important for joint replacement clients but also for general fitness, performance, and pain clients! Begin learning a neuro-centric approach to medical fitness and how to work with joint replacement clients with our Joint Replacement Fitness Specialist online course, available through the MedFit Classroom!
Pat Marques is a Z-Health Master Trainer and NSCA-CPT specializing in training the nervous system to improve performance and get out of pain. After retiring from the Active Duty Army, Pat pursued his education and certifications in exercise science, initially working with wounded, ill, and injured soldiers. During this time that Pat discovered the power of using a neurological approach to training to get out of pain and improve fitness and performance. He currently provides exercise therapy, movement reeducation, and strength and conditioning for all levels of clients at NeuroAthlete, from chronic pain sufferers to Olympic-level and professional athletes.
References
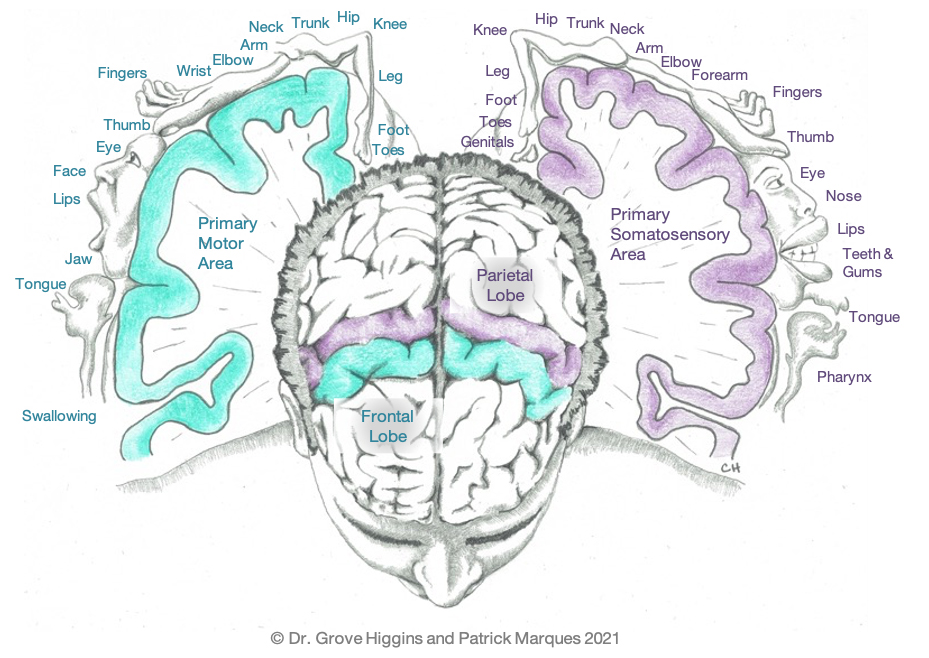
In our previous article, we showed you this picture to help understand neuroplasticity and how neurons that wire together, fire together. In this blog we’ll use the same picture to understand how sensory input to the brain affects motor output.
The sensory area (purple) is on the front “slice” of the parietal lobe. The neurons here will be activated by sensory input such as touch, vibration, threat, pressure, temperature and joint position. Lying just in front of the sensory area is the motor area (blue), which is the back “slice” of the frontal lobe. The neurons here are activated through volitional movement.
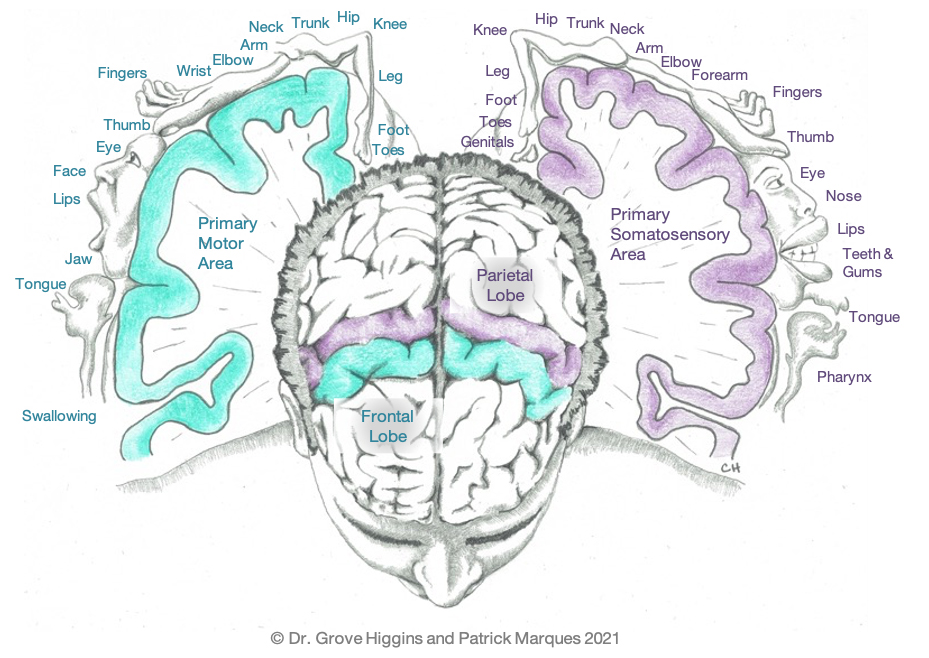
In both the sensory and motor areas of the brain, you can see in the illustration that specific areas are dedicated to specific body parts. And those areas are represented in the same areas for sensory and motor (e.g., where the hand is located in the sensory area is in the same place in motor area along the “slice”).
The bottom line is that for you to move an area well, your brain must be able feel, or “sense”, the area well. This is why issues like peripheral neuropathy in the feet so greatly affect the ability to balance and walk. Having good sensory input from an area of the body is a prerequisite for good motor control when we try to move an area.
One of the most prominent dysfunctions after stroke is a reduced ability to move one side of the body. This can occur at many different levels, from total paralysis to reduced coordination of fine motor skills. Common examples include limb spasticity, usually in flexion (e.g., a clenched fist held close into the chest), or what is termed “drop foot”, an inability to dorsiflex (lift) the foot, which severely interferes with a safe, functional gait pattern. This happens because the stroke damaged areas in the motor cortex associated with the affected body part.
The good news is that by increased sensory input to the affected area, we can begin to improve motor output. You have likely seen this already if you have ever used things like percussion guns or kinesiology tape. The many new “toys” we see in the fitness industry these days are simply sensory input devices, providing the sensory area with more and novel input, which then allows the motor area to “fire” better and provide better movement (i.e., improved range of motion, more strength, etc.).
A 2017 study found that “kinesio tape application to the tibialis anterior has significant effects on motor recovery of the lower extremity, spasticity, ambulation capacity, HRQoL (health-related quality of life) and gait compared to the control group and baseline.” (1)
The concept of sensory input affecting motor output and how to harness it is not only for stroke recovery, but also for general fitness, performance, and pain clients!
Begin learning a neuro-centric approach to medical fitness and how to work with stroke survivors with our Stroke Recovery Fitness Specialist online course, available through the MedFit Classroom.
Pat Marques is a Z-Health Master Trainer and NSCA-CPT specializing in training the nervous system to improve performance and get out of pain. After retiring from the Active Duty Army, Pat pursued his education and certifications in exercise science, initially working with wounded, ill, and injured soldiers. During this time that Pat discovered the power of using a neurological approach to training to get out of pain and improve fitness and performance. He currently provides exercise therapy, movement reeducation, and strength and conditioning for all levels of clients at NeuroAthlete, from chronic pain sufferers to Olympic-level and professional athletes.
References