Key Exercises and Training for Aging Successfully and Living Your Best Life
As the years roll by, nothing has become clearer to me than the fact that aging successfully requires a lot of work. When it comes to our bodies, nothing rings truer than, “If you don’t use it, you lose it.” This is particularly true not only when it comes to preventing declines arising from disuse, but also when trying to slow down the normal impacts of aging.
The function of our bodily systems peaks at around age 25 and declines over time. As a result, your maximal aerobic capacity decreases, even with constant training, reflective of declines in maximal heart rate. In addition, your balance ability gets worse (particularly after age 40), bones get thinner, muscles atrophy, reflexes get slower, and recovery from workouts takes longer. Aging is not for sissies, but it beats the alternative!

The good news is that it is possible to slow the rapid decline of these systems by changing how you live your life. By including regular physical training, better nutrition, adequate sleep, and stress management, you can delay or prevent a lot of normal aging and reverse decrements caused by inactivity, neglect, disuse, and abuse of our bodies. The only caveat is that we can’t control or reverse neurological decline.
It starts to seem like preventing additional declines from inactivity or inadequate training gets to be a full-time job as you get older and you have to keep adding in additional exercises, stretches, and activities. A fitness instructor recently confirmed that it’s a bit like playing whack-a-mole: fix one weak area or physical problem and another one pops up. Welcome to aging!
So what can you do to live your best life both physically and mentally? I would suggest adding at least these (and many other) critical exercises to your weekly routine:
Cardiorespiratory fitness: Cardio workouts with faster training intervals
In addition to doing regular cardio activities like walking, cycling, and swimming, add in some faster intervals into any workout, such as walking faster for 10 to 60 seconds at a time during your normal walk or doing a hill profile on a cardio training machine. Doing so will increase your fitness more and improve insulin sensitivity for longer. It’s also fine to do high-intensity interval training (HIIT) at least once a week, but start out slowly and progress slowly to prevent injuries and demotivation. Not all your workouts should be equally intense, and varying your aerobic activities also lowers the risk of getting injured.
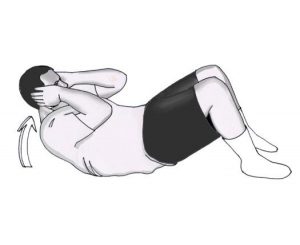
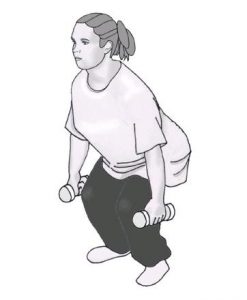
Muscular strength and endurance: Resistance training exercises
It is easy to work on your muscle strength and muscle endurance by doing a series of resistance exercises targeting your major muscle groups (in the upper body, lower body, and core areas). Pick at least 8 to 10 exercises that cover all these areas and do them at least two to three days per week. It’s fine to use your own body weight, household items (like full water bottles), hand weights, or resistance bands as resistance—you don’t have to have access to a gym or leave home. Adding in these exercises to your weekly routine is critical to aging well and being able to live independently throughout your entire lifespan.
Balance ability: Standing on one leg at a time (and other balance exercises)
This simple exercise involves standing on one leg for a minute, switching to the other leg, and repeating. Have something you can grab onto nearby, such as the back of a chair. You can hold on with both hands, one hand, one finger, or nothing as you get better at balancing. To challenge yourself, move your free leg in different directions (e.g., out front, to the side, behind you) while standing on the other one, or practice standing on uneven surfaces, such as a cushion. If your balance ability is really getting to be an issue, include other balance training activities each week as well.
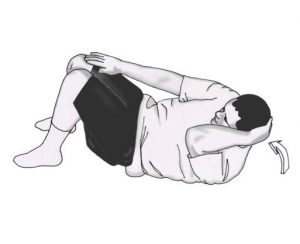
Joint mobility and cartilage health: Stretches for all your joints
Do a series of flexibility exercises that stretch your joints in all their normal directions to maintain and increase their range of motion. With aging, we are all losing flexibility and diabetes can accelerate this loss when extra glucose sticks to joint surfaces (cartilage) over time and makes them more brittle. Try to stretch at least two to three days per week. The older you get, the longer you should hold each stretch (up to a minute on each one), and you may need to add in specialized stretches (such as for your calves or hips) to really work tighter joints to enhance your mobility and balance ability.

Bone strength: Weight-bearing activities and/or resistance training exercises
Your bones stay stronger when you put normal stress on them regularly, such as carrying your own body weight around when walking or jogging or doing resistance exercises with your upper body or carrying grocery bags. If you stay sedentary, your bones will lose minerals faster and get thinned out more quickly, and non-weight-bearing activities like swimming and cycling just don’t have the ability to build bone as much as weight-bearing ones. Try to adequately stress your bones to stimulate the bone mineral density to stay higher—at least two to three days per week.
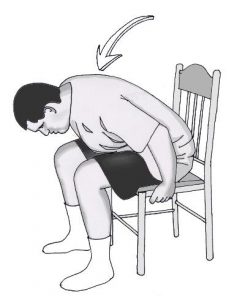
Basic mobility and self-care: Wall sits and/or sit-to-stand exercise
Until you start to get older, you seldom think about how difficult it can be to get up out of a chair or off the sofa. Many older people get heavier and weaker and start to have trouble doing these basic maneuvers, which are critical to living well independently. To improve your ability, practice doing wall sits, which involves sitting against a wall with your hips and knees at 90 degree angles and your feet straight below your knees for as long as you can. This exercise will also help prevent knee pain and problems. Alternatively, you can do sit-to-stand exercises where you sit on the edge of an armless chair and practice getting up without using your arms. (This is also often called the “getting up from the toilet” exercise.)
Sexual enjoyment (and incontinence): Kegel exercises
Also known as pelvic floor muscle training, Kegel exercises can help with stress incontinence (i.e., urinating a little when sneezing or laughing) and normal incontinence (both urinary or fecal), and they may enhance your sexual pleasure to boot. The easiest way to identify the pelvic floor muscles is to stop your urine flow while urinating or tighten the muscles that keep you from passing gas. To do Kegels, imagine you are sitting on a marble and pretend you’re lifting it up by tightening your pelvic muscles and holding them contracted for as long as you can; do this a few times in a row. When your muscles get stronger, you can do these exercises while sitting, standing, or walking. Both men and women can and should do Kegel exercises regularly.
Sheri R. Colberg, PhD, is the author of The Athlete’s Guide to Diabetes: Expert Advice for 165 Sports and Activities (the newest edition of Diabetic Athlete’s Handbook). She is also the author of Diabetes & Keeping Fit for Dummies, co-published by Wiley and the ADA. A professor emerita of exercise science from Old Dominion University and an internationally recognized diabetes motion expert, she is the author of 12 books, 34 book chapters, and over 420 articles. She was honored with the 2016 American Diabetes Association Outstanding Educator in Diabetes Award. Contact her via her websites (SheriColberg.com and DiabetesMotion.com).


















 Many people are stuck at home for one reason or another think they can’t work on staying fit, but the truth is that you can get a stronger core and stay fitter without leaving home. You’d be amazed at how easy it is to get your fit on.
Many people are stuck at home for one reason or another think they can’t work on staying fit, but the truth is that you can get a stronger core and stay fitter without leaving home. You’d be amazed at how easy it is to get your fit on.