Introduction
Muscle aches and pain are common in all of us, despite the type of work, activity or the cumulative activities we do. Once thing is for certain, as an experienced physical therapist, I have seen something unique. Patients who complain with an increase in pain, and trigger points present, despite if they had surgery, trauma, increased stress in their lives or have been suffering from chronic pain. One of the most common types of pain is fibromyalgia. This article will review the background on fibromyalgia, clinical presentation & pathology, the medical and physical therapy treatment approach. Provide the latest evidenced based research on treating fibromyalgia, but more importantly, how to work with a fibromyalgia client using effective programming and periodization training principles guiding the personal trainer to help the client reach optimal goals safely and based on science.
Background
The literal translation of fibromyalgia comes from “fibro” meaning fibrous tissues (such as tendons and ligaments), “my” meaning muscles, and “algia” meaning pain. Fibromyalgia syndrome (FMS) has an estimated prevalence in North America and Europe of 0.5% to 5.8%. According to the criteria of the American College of Rheumatology (ACR), FMS is defined as chronic widespread pain and tenderness at a minimum of 11 of 18 points, defined as tender points, that last longer than 3 months in duration(Häuser, W., et al, 2009).

Figure 1. Stiffness associated with pain
What is Fibromyalgia?
Pathophysiology: Individuals suffering from fibromyalgia display enhanced sensitivity to a wide array of stimuli, such as heat and cold, as well as to mechanical and ischemic pressure.
Trigger points are areas of where the muscle shortens, which clinically we call adaptive shortening.
There trigger points are areas of “hyperexcitability,” which contain irritants (bradykinin, substance p, cytokines) that are stored within the trigger point. These irritants develop by stress, trauma, poor posture, just to name a few. Physiologically the muscle fibers actin and myosin become shortened, and less efficient to move and slide within the muscle, thus affecting movement.
Contributing factors: Factors contributing to the pathophysiology of fibromyalgia include abnormal function of the autonomic and neuroendocrine systems, genetic influences, and other triggers such as stress, anxiety, fear, anger and other emotional variables (Bradley, L, 2009).
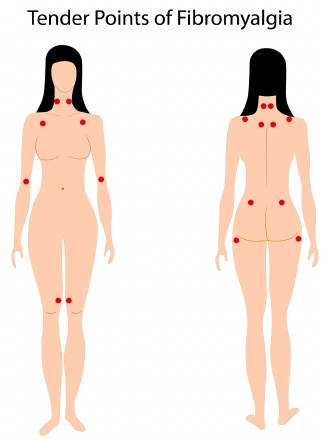
Figure 2. Common locations of tender points associated with Fibromyalgia
Sign and symptoms: According to the criteria of the American College of Rheumatology (ACR), fibromyalgia syndrome (FMS) is defined as chronic widespread pain and tenderness in at least eleven of 18 defined tender points (Häuser, W., et al, 2010). FMS is frequently associated with fatigue, sleep disorder, mental and physical disorders, as well as disability and diminished quality of life. With fibromyalgia, a person will have feel stiff and achy, particularly in the morning that improves during the day and is sore by the end of the day.
Associated symptoms: Patient may present with central sensitization. Central sensitization is when persistent nocioceptive input leads to increased excitability in the dorsal horn neurons
of the spinal cord. Other symptoms of FMS are fatigue and disrupted sleep.
Medical management: Several high level randomized control trial articles, have shown there is
Strong evidence that anti depressants reduce pain. However, there are other interventions that are very effective per the research (Häuser, W., et al, 2009).
Cognitive therapy is based on the premise that modifying maladaptive thoughts results in changes in both affect and behavior. High level research or meta-analysis has shown that cognitive behavioral therapy (CBT) has significant effectiveness in treating associated symptoms of depression, and anxiety, which is common with patients who suffer from Fibromyalgia. In addition, research shows that relaxation techniques have also proven to be helpful for FM symptoms include, but are not limited to, progressive muscle relaxation, autogenic training, guided imagery and meditation (Hassett, A., & Gervirtz, R., 2009).
The term “Qigong” generally describes a number of traditional Chinese therapies and exercises all believed to facilitate the flow of vital energy or “chi.”
Physical therapy: Patient education is the most important element in helping a fibromyalgia patient. Understanding that utilizing a comprehensive approach is the most effective and a must, to manage and improve one’s quality of life.
Manual therapy is one of the most effective approaches to address the stiffness a fibromyalgia patient presents with by using a manual therapy approach. Myofascial release and soft tissue massage are two manual therapy approaches that not only relax the patient, but enable the therapist to improve the elasticity of the muscle, whereby effecting the actin and myosin to improve Their ability to contract and lengthen during functional movements. Stretching the upper trapezius, lumbar, specifically the quadratus lumborum, the iliotibial band, legs and calves are Important to restore optimal muscle length for movement.
Aqua therapy is very effective per the research. In a study by Diego, I., & Legaz-Arrese, A., (2008), wanted to evaluate the effects of a 16-week exercise therapy in a chest-high pool of warm water through applicable tests in the clinical practice on the global symptomatology of women with fibromyalgia (FM) and to determine exercise. The intervention was a 16-week aquatic training program, including strength training, aerobic training, and relaxation exercises. Results: those patients who were involved in the strength training, aerobic training and relaxation group, showed significant deficiencies compared with the healthy subjects. The group had significant decrease in the tender point, improving sleep quality, cognitive function, and physical function.
Massage can very effective to compliment physical therapy reducing tension, trigger points, whereby improving relaxation to the body. Cross training such as hiking and walking are all part of the “organic” approach to help the FM patient achieve optimal wellness.
Recommendations For Training
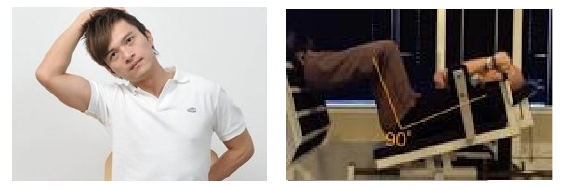
Left: Figure 3. Stretching upper trapezius; Right: Figure 4. Stretching thoracic area
Training a FM client should involve mild intensity and as always, should be specific to the goals of the client. Strength training should focus on weaker phasic muscles such as; glute maximus, glute medius/minimus and hamstrings>quadriceps. The choice of exercise and type of equipment depends on several factors; the client’s experience with exercise, time, body type, goals and whether or not the client had or underwent surgery.
Stretching should focus on upper trapezius and neck musculature where the tender points typically are in the upper torso as seen in figure 3 and 4. Strengthening should focus on strengthening the weaker rhomboids (through mid row exercise), low trap pull downs, seated reverse flyes and targeting weaker glute medius, glute minimus and glute maximus muscles.
A simple beginning exercise is the horizontal leg press, which targets the hamstrings and glute maximus primarily. This can be progressed to diagonal lunges, which target the weaker glute medius and glute minimus musculature.

Figure 6. Trunk rotation w/medicine ball with in place lunge
Core stabilization training should focus on weaker phasic external oblique, quadratus lumborum and multifidi. Exercises such as bridging with ball, standing trunk rotation with cable or medicine ball, progressed to partial lunge with trunk rotation with medicine ball is ideal. Cross training with yoga and pilates can not only improve flexibility and breathing but core strength in multi directions and progressed as appropriate. Swimming also can serve to compliment training due to the buoyancy principle and how relaxing it can feel.
Summary
Fibromyalgia (FM) can be devastating to deal with. Throughout my career as both a physical therapist and personal trainer, I have treated a large amount of patients with mild, moderate to severe fibromyalgia. I use a personalized approach treating patients with FM similarly to training clients with FM.
Fibromyalgia is a chronic musculoskeletal pain syndrome that is associated with a wide variety of symptoms, significantly affecting daily function, making exercise very discouraging.
Fitness professionals can make a significant positive impact on a client with fibromyalgia. It first begins with understanding the science behind the dysfunction, listening, observing, modifying and designing programs that are based on science. Utilize appropriate programming and periodization training principles is fundamental. Training a client should focus on reducing stress, improving flexibility, strengthening that is client specific and including core training and cross training that is upbeat and delivers sound results.
Chris Gellert, PT, MMusc & Sportsphysio, MPT, CSCS, AMS is the CEO of Pinnacle Training & Consulting Systems(PTCS). A continuing education company, that provides educational material in the forms of home study courses, live seminars, DVDs, webinars, articles and min books teaching in-depth, the foundation science, functional assessments and practical application behind Human Movement, that is evidenced based. Chris is both a dynamic physical therapist with 15 years experience, and a personal trainer with 19 years experience, with advanced training, has created over 10 courses, is an experienced international fitness presenter, writes for various websites and international publications, consults and teaches seminars on human movement. For more information, please visit www.pinnacle-tcs.com.
REFERENCES
Bradley, L, 2009, ‘Pathophysiology of Fibromyalgia,’ American Journal of Sports Medicine, vol. 22, issue 12, pp. 1-9.
Diego, I., & Legaz-Arrese, A., 2008, ‘Assessment of the Effects of Aquatic Therapy on Global Symptomatology in Patients With Fibromyalgia Syndrome: A Randomized Controlled Trial,’ Archive of Physical Medicine Rehabilitation, vol. 89, pp. 225-2256.
Hassett, A., & Gervirtz, R., 2009, ‘Nonpharmacologic, ‘Treatment for Fibromyalgia: Patient Education, Cognitive-Behavioral Therapy, Relaxation Techniques, and Complementary and Alternative Medicine,’ Rheum Disorders Clinical North America. Vol. 35, issue 2, pp. 393–407.
Häuser, W., et al, 2009, ‘Treatment of Fibromyalgia Syndrome With Antidepressants: A Meta-analysis,’ vol. 301, issue 2, pp. 198-209.
Häuser, W., et al, 2010, ‘Review Guidelines on the management of fibromyalgia syndrome – A systematic review’ European Journal of Pain, Issue 14, pp. 5–10.
Sanchez, A., et al., 2011, ‘Effects of myofascial release techniques on pain, physical function and postural stability in patients with fibromyalgia: a randomized controlled trial,’ vol. 25, issue 9, pp. 800-813.
