The Importance of Exercise for the Disabled or Handicapped
Everyone must remain active. This is only achievable with the help of exercise. Contrary to popular belief, handicapped people also wish to stay fit and healthy. On the other hand, some of handicapped individuals do not realize the importance of it.
Let’s discuss the importance of exercise for handicapped people.
Prevention of Heart Disease
Exercise can help reduce the risk of developing diseases relating to the heart. This includes high blood pressure, heart attack and ischemic heart disease. Furthermore, exercise is essential for preventing various other medical conditions.

Prevention of Comorbidities
Inactivity is a disease in itself. Being inactive makes the body less productive. This makes them more prone to the development of illness, ranging from something as small as flu to as big as cancer. Disabled and inactive individuals have a higher chance of developing colon cancer and diabetes.
Prevention of Anxiety and Depression
Being inactive and indoors can lead to depression and anxiety. You may feel down most of the time. Exercising releases endorphins in our body. These help in regulating mood; those who exercise regularly experience improvement in their moods.
Alleviates pain
Inactivity can cause harm to your bones and muscles as well. The majority of people suffer from pain in joints and other complications. Stiff muscles are also an additional drawback of inactivity.
Handicapped people who exercise more often do not suffer from these symptoms. They report relief of pain. Furthermore, such people also have faster healing of wounds and injury from trauma.
Clears the mind
Exercising not only helps with our physical well-being. It also aids in improving our mental health as well. Brain fog is a real thing; people can be doubtful about the decisions they make. Exercising helps people to think clearly. They can divert their mind from useless jargon to more productive thoughts.
DO NOT LET OTHERS STOP YOU FROM EXERCISING
Being handicapped has a certain societal stigma with it. The perception of people can often stop you from exercising. Always remember that exercising will only benefit you alone. Don’t worry about what others think!
Conclusion
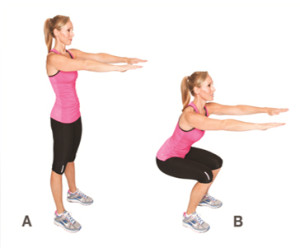
Being disabled can be a hard thing. But, exercise is an activity that will help you to gain self-esteem. You do not need to start with rigorous workouts.
This journey begins with a single step, time will help you get better in the long run. So what are you waiting for? Start looking for an exercise regimen that suits you best.
Here’s to your health!
Terrance Hutchinson is the Owner of Your Best Lifestyles Fitness and Nutrition. He is a Certified Personal trainer specializing in Exercise Therapy, Corrective Exercise, Sports Nutrition, and Corporate Wellness. He an author of 3 books, he has his own podcast, he has contributed articles to major newspapers and magazines, Terrance has spoken at health events, webinars, seminars, hospitals, schools, doctors offices and has been featured nationally syndicated television platforms. Terrance has clients in many states and counties and is looking to help others bridge the gap between the medical and fitness industries. To learn more about Terrance, visit yourbestlifestyles.com