Patients Need Personal Trainers: How personal training can impact millions
In the United States, 11.2 million people were diagnosed with obesity and/or diabetes over the last year.(1,5) These are primary risk factors leading to stroke and total joint replacements, adding another 8 million people per year.(6,7) This means that the fitness professional in the post-medical and post-rehabilitation space has more potential clients than they could hope to serve. The question is how to reach them and build a business around these problems.

Personal Trainer and marketer Joe Lemon has some advice. Two primary problems for trainers trying to innovate this post medical/rehabilitation space are trust and visibility. Both these problems are interrelated and so deserve to be tackled for this space to become profitable.
In the United States, less than 50% of physicians suggest patients go to a gym. Even less (20%) recommend a personal trainer.(4) But the question is, why? First, we found a general ignorance of what personal trainers can do for their clients and, secondarily, if personal training was a safe, effective modality. This is partially due to a lack of standardization in personal training education and regulation across the USA. In addition, until recently, there has been a lack of specific training for fitness professionals in the medical fitness space that can be understood and trusted.
Even for those exceptional personal trainers who do provide the training to address specific clients’ post-medical/rehabilitation needs, there is a gap between their skills and clinicians’ knowledge that they exist. Joe has practical advice to close that gap and create a bridge to clinicians.
First, identify who these clinicians are. Sports medicine, orthopedic surgeons, neurologists, bariatric doctors and primary care physicians are all viable referral sources. Network and get to know someone who can make personal introductions for you directly to the doctor or their assistant or office manager, who is often the gatekeeper of the practice. Once you get the opportunity to talk to them, give them tangible, always take a pamphlet explaining your qualifications, education, and process. Providing them with hard copy printouts from the MedFit websites (medfitnetwork.org and medfitclassroom.org) are the most accessible sources of information you could use. And always, leave them with the material they can give their patients that link directly back to you in the form of business cards and pamphlets/brochures.
Lastly, get out and talk about what you do. Remember, communication is 7% what you say where 38% how you speak it, and 55% your body language.(3) Getting in front of people these days is easier now than ever. Schedule talks at gyms and coffeehouses, video it, and post it online. The more you talk passionately about what you love doing, the better. Connect with your potential client recruit them to be your spokesperson to their physician for you.
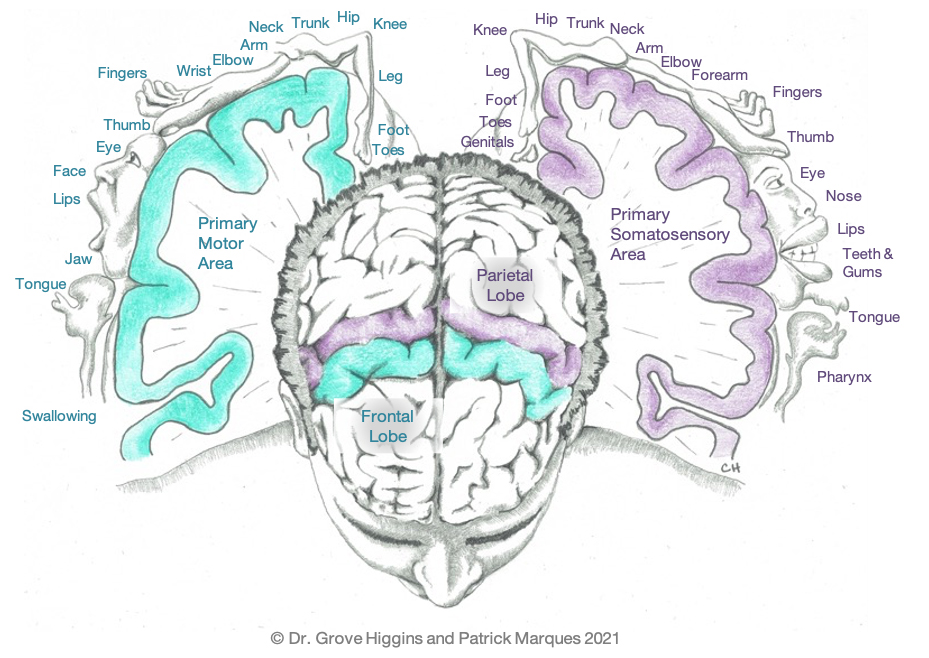
Dr. Grove Higgins is a chiropractor, rehabilitationist, soft tissue injury expert, researcher, anatomy instructor, biomechanist, human performance expert, speaker, and corporate health consultant. In 2015, Dr. Higgins cofounded Neuroathlete with Coach Patrick Marques (LTC, US Army Ret.) and Peter Hoversten. Neuroathlete’s goal is to more broadly deliver neurological training to a global audience.
References
- (CDC), U. D. (2021). 2020, National Diabetes Statistics Report.
- Lemon, J. (2021). Business Development, Market Research, & Strategic Partnerships. (G. Higgins, Interviewer)
- Michail, J. (2020, 8 24). Strong Nonverbal Skills Matter Now More Than Ever In The “New Normal”. Retrieved from Forbes: https://www.forbes.com/sites/forbescoachescouncil/2020/08/24/strong-nonverbal-skills-matter-now-more-than-ever-in-this-new-normal
- Pojednic, R., Bantham, A., Arnstein, F., Kennedy, M., & Phillips, E. (2018). Bridging the gap between clinicians and fitness professional: a challeng to implimenting exercise as medicine. BMJ Open Sport & Exercise Medicine, 1-5.
- CDC f. (2021, 3 1). National Center for Health Statistics. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/nchs/hus/contents2019.htm#Table-021
- Springer, B. D. (2021). Highlights of the 2020 American Joint Replacement Registry Annual Report. Arthroplasty Today, 9, 141-142.
- Stroke. (2021, 5 25). Retrieved from Center for Disease Control and Prevention: https://www.cdc.gov/stroke/facts.htm






 However, many trainers fall in love working with these clients, whether they are a
However, many trainers fall in love working with these clients, whether they are a