Grip Strength for Everyday Function: From Hands to Forearms
What is the role of grip strength in daily activities and overall health?
Lost your password? Please enter your email address. You will receive a link to create a new password.

What is the role of grip strength in daily activities and overall health?
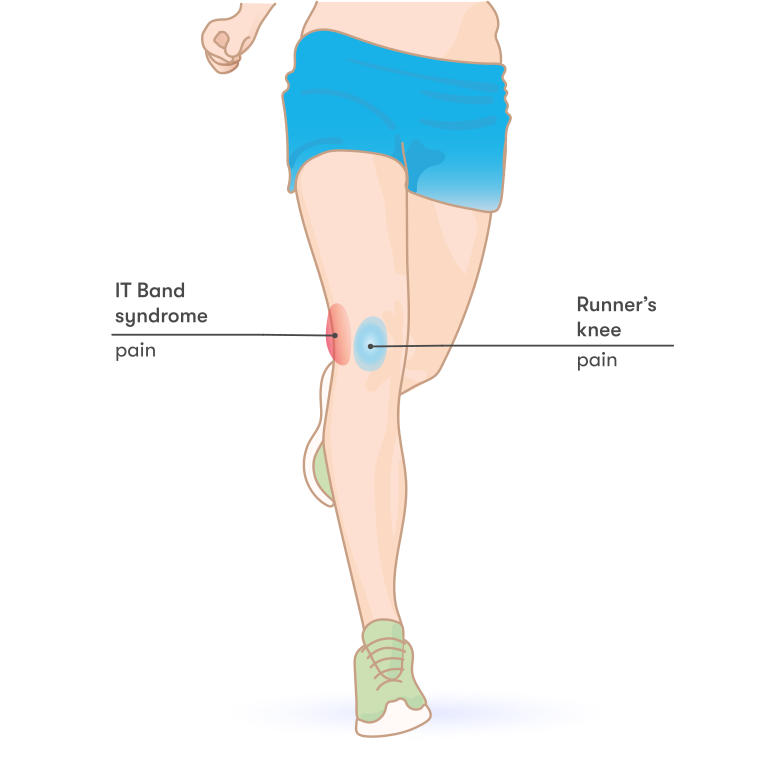
Iliotibial band syndrome (IT) is a pain many workout enthusiasts, runners, and cyclists can experience.

*Before we begin, it is essential to look at your accrediting agency’s ‘Scope of Practice.’ Remember, as a Certified Personal Trainers, we DON’T diagnose, prescribe, treat injury or disease, rehabilitate, counsel, or work with patients. We DO perform fitness screenings, design exercise programs, coach, give general health information, refer clients to medical health professionals when needed, and work with clients.
I have been a personal trainer for over 30 years and have had clients with me for decades. You cannot work that closely for that long with human beings and NOT come across a crisis.

How do we define “Crisis”? The dictionary defines crisis as a time of intense difficulty, trouble, or danger. It includes but is not limited to death, divorce, health scares and medical diagnoses, job loss, financial struggles, family struggles, mental health journeys, injuries and illness, surgeries, car accidents, and so on.
The research is solid.
Exercise is proven to release positive endorphins and happy hormones. Exercise can be a tremendous stress and anxiety release. Exercise will not FIX the crisis but is an excellent way to cope with the problem, clear the mind, and settle the body to be in a better place to navigate the situation.
The good news is as personal trainers, we have a unique opportunity to be in the room where it happens. Physical exercise can be very cathartic for clients going through difficult situations. I cannot count the times I have had a client break down and cry in our sessions. In my own experience, numerous doctors and friends recommended I start yoga classes when dealing with high anxiety. I walked into a class taught by one of my dearest friends and almost had to leave because I was sobbing so audibly I was afraid to disrupt others’ experience. Something unlocked in me during that class. Yoga did not fix my situation or my anxiety, but it did help me navigate my situation better and soothe it for the time being.
I count it a privilege to walk alongside my clients when they are going through a crisis. But it is essential to do so professionally and avoid getting tangled in their situation yourself.
There is a visual picture that many supporting agencies or groups use when training to work with people in crisis that can also be helpful to personal trainers. The image is a large pit or hole in the ground, and the person in crisis is at the bottom of the pit and cannot get out on their own.
The dilemma is how to help that person without getting pulled down in the hole with them, but instead giving them the assistance and support to get themselves out of the hole.
Initially, we should provide a safe place for our clients to share what life is offering them at that time. It is crucial to their physical health and can affect their performance during the training sessions.
Avoid judging the story and offering advice, but rather asking questions. “What do you think is the next step to solve this issue?” Often our clients want to be heard and seen. Giving them the space to share can often lead them to the solution or the next step or provide them with the freedom to move through the grieving process, whatever the situation may be. Of course, direct your client to professional help if you feel they are in danger or experiencing extreme levels of depression, anxiety, or hopelessness. You should have referrals on hand for anything a client needs outside of your Scope of Practice! It takes a village to keep our health in check.
How do we do this and still train our clients? I certainly do not intend for you to have an hour-long listening session instead of training them. Quite the contrary; the training will help them through the crisis.
Here are some of my tricks:

You can be the missing puzzle piece that helps get them through.
It is a fine line between ushering your client through crisis and getting involved in their situation, but it can be done, and one size doesn’t fit all. Find the things that work for you and your client. But see them, hear them, and continue to point them to the positive benefits of working out during a difficult season of life. Their physical and mental health will benefit dramatically. It may not be the time to set huge fitness goals, but maintaining their fitness, assisting their immune system under intense stress, and helping with sleep during these times are critical to success.
In closing, I said earlier that I am privileged to walk with my clients through a crisis. And my favorite part of my job is seeing the light at the end of the tunnel. Then celebrate with them when the situation is over, or the grieving is complete. Don’t forget to point out how strong they are, how resilient they are, and not only where they were but how far they have come!
Shannon Briggs is a multi-passionate fitness professional and educator. She brings 30-plus years of experience in the dance and fitness industry. Shannon is the Personal Trainer to the Kilgore Rangerettes and helps Collegiate Fitness and Wellness Directors fill in the gaps. She leads continuing education workshops in multiple group fitness formats and topics specific to personal training.

You’ve heard the terms functional exercise, functional movement or functional movement patterns… but what do these terms actually mean?
The term “functional movement patterns” is confusing because it is really not a specific term. Trainers, especially those putting MSers on exercise programs, will usually take them through a program of upper and lower body exercises incorporating compound movements that ask your body to do several things at once. They tell you this is a functional exercise routine and that it’s the best way to help you with your MS limitations. Every exercise is NOT considered a functional one. So what’s the difference?
Functional, by definition, means, “of or having a special activity, purpose, or task; relating to the way in which something works or operates”. In this case, the task is being a functional MSer with the ability to use your body to do what you’d like it to do like you did before your MS diagnosis.
And even though being “functional” is different from one person to the next—for instance, a triathlete needs to be able to run, bike, and swim without limitation or pain, while a homemaker (male or female) needs to be able to do household chores such as lifting groceries out of a car, moving a vacuum cleaner and loading and unloading a dishwasher without limitation or pain—the actual movement patterns required for these activities aren’t really that different.
When you think of functional movement patterns, you should see them as movements that engage your whole body in a variety of different active ways that involve coordinating your upper and lower body with areas that alternate from being steady to moving, and back again.

So where exercises like squats are considered functional because they require full-body coordination, strength, and stability exercises like biceps curls aren’t considered functional because they lack the full-body mental and physical engagement that comes into play with basic motion.
The main difference between functional training and other exercises that work each muscle is that exercises such as biceps curls or leg extensions attempt to isolate that muscle. When doing these movements we’re working individual body parts as separate from the others creating stimulus within those parts. Functional movements put the emphasis on using your whole body at once.
The focus on functional movement patterns, in theory, is to train your body to move effectively as a fully connected single unit so it is able to sit, stand, bend or change direction effectively when you need it to. Some of the functional exercises I use are squats, lunges, and pushups. These movements effectively engage the whole body in the exercise although they emphasize specific muscles as the main force of action.

I believe in functional movement patterns and agree there is a place for them in MS training BUT without the individual muscle-specific training it would be impossible to do a functional movement. If your legs are so weak from MS limitations how are you going to perform a proper squat that uses all the muscles in your legs?! You won’t be able to. This is why specific muscle training is so important. And the only way to get muscle-specific strength is through resistance training. But it doesn’t end there…
You must strength train each major muscle group, individually and specifically to gain the ability to “function”. I know you keep hearing about functional exercise for MS and how important it is. You are told that you MUST be in a program using functional movement patterns to help your MS limitations. I HAVE MS and I have been a fitness expert for more than 40 years. The real FACT is that functional movement patterns are secondary to strength training. They are important but more important to your physical abilities are training methods that incorporate resistance exercises with principles that cause “thought-based training” ™ which create muscle fiber activation, neuroplasticity, and brain to muscle reconnection.
Please be careful with who and what you take in as being the right fitness information for MS, especially coming from fitness “experts” who do not understand MS. There is much more to proper exercise for MS than jumping into the next repetitive functional program. And any trainer who says he/she is teaching you how to place mental attention on your workouts but only tells you to concentrate on what you are doing does not understand the significance of proper focus. It is not just a simple matter of paying attention to your exercises and form. It is the training methods you use that force that focus and concentration that is of key importance in your MS exercise program. Exercise programs pushing functional pattern movements with no focus driven process or training method behind them other than the standard and cookie-cutter, “do 10 reps of 3 sets”, are of little value in bringing results to our MS bodies.
Learn what you need to help MSers… check out the Multiple Sclerosis Fitness Specialist online course for fitness and health professionals!

David Lyons, BS, CPT, is the founder of OptimalBody, which touches the lives of fitness enthusiasts of all kinds. OptimalBody has been named The Most Comprehensive MS Fitness Program worldwide since its release. His book, Everyday Health & Fitness with Multiple Sclerosis, was a #1 New Release on Amazon at its release. He is the 2013 recipient of the Health Advocate of the Year Award; in 2015, he received the first ever Health Advocate Lifetime Achievement Award, and the Lifetime Fitness Inspiration Award in Feb 2016. In 2017, David received the Special Recognition Award from the National Fitness Hall of Fame.

Overly stretched, tiny tears can lead to inflammation and pain in the arch of the foot. This condition, called plantar fasciitis, accounts for nearly one million doctor visits per year. Our foot has a thick band of tissue called fascia that runs from our heel to our toe. This troublesome foot issue is actually more common in women than men. We need to spend time on our feet moving, so this foot problem, if left untreated, can cause excessive pain and greatly limit our mobility.
Plantar fasciitis is more common as we age (specifically between ages 40 and 60), but is also more likely to occur in someone who is overweight or constantly on their feet. It is very common in runners. Activities that are known for high rates of plantar fasciitis include ballet, dance, long-distance running, and ballistic jumping. There are a few other contributing factors which include wearing shoes that are worn out and have thin soles or wearing high-heels. The mechanics of how you walk (your stride) involves your foot position. If you have flat feet or a tight Achilles, the body will compensate for these dysfunctions which can lead to injury of the fascia.

Pain starts to occur near the heel towards the bottom of the foot. Most people feel the pain in the morning right when they get out of bed. This is known as “first-step pain”. This can also occur if you have been sitting for a long period of time and then stand up. The plantar fascia acts like an absorbing shock spring in our foot. Repetitive stretching and tearing of this area results in a stabbing pain.
If pain persists, seeing a doctor can help detect this condition. He or she will check the tender areas of the foot. The good news is that plantar fasciitis does normally go away on its own. There are several treatment options. A doctor might prescribe anti-inflammatory medication or a steroid injection. Physical therapy and massage can help as well as shock wave therapy to stimulate blood flow. A Tenex procedure can remove scar tissue in the area or surgery can be done to remove the plantar fascia off of the heel bone. Wearing the right shoes or using shoe inserts oftentimes does the trick, so be sure to try these simple fixes first. Ice and soaking the heel can also help alleviate pain .
A good home remedy is freezing a foam cup of water then rubbing the top of the cup on the heel for 10 or so minutes. Stretching the calves and Achilles tendon can help over time and there are ways to tape the area of the foot to position the heel correctly with each step. Night splints worn to hold the foot at a 90 degree angle help when stretching the fascia.
There’s no doubt that we use and abuse our feet, bearing vast amounts of weight on them while performing all of our daily functions. As we walk from point A to point B, getting those 10,000 steps in, we must practice self-care from head to toe to heel. Sometimes foregoing that cute pair of shoes even at the gym is worth the fashion sacrifice to walk without pain.
Megan Johnson McCullough, owner of Every BODY’s Fit in Oceanside CA, is a NASM Master Trainer, AFAA group exercise instructor, and specializes in Fitness Nutrition, Weight Management, Senior Fitness, Corrective Exercise, and Drug and Alcohol Recovery. She’s also a Wellness Coach, holds an M.A. Physical Education & Health, and is a current doctoral candidate in Health and Human Performance. She is a professional natural bodybuilder, fitness model, and published author.
References
https://journals.lww.com/jaapa/Fulltext/2018/01000/Plantar_fasciitis__A_review_of_treatments.4.aspx
https://journals.sagepub.com/doi/full/10.1177/2473011419896763
https://academic.oup.com/occmed/article/65/2/97/1488760

Let’s discuss the relationship between narcissism and the fitness world and examine why those working in this demographic need to identify and be aware of narcissistic behaviors, not only in themselves but others.

You may have heard people warn that pregnant women shouldn’t raise anything over their heads or lift objects that are heavier than ten pounds when pregnant. These are warnings that still make the fitness trainer rounds when working with pregnant clients, yet these warnings aren’t based on science. In fact, there’s no evidence for warning pregnant women to avoid lifting over their head unless it causes discomfort or balance issues, and the ten-pound limit is even more questionable, as ten pounds would be too heavy for some women and as easy as a feather for others.

It’s important to always remember that each pregnant woman has a specific fitness level and ability, so setting arbitrary limits is an ineffective way to provide guidelines for this population. In addition, when confronted with statements such as these, always review the research that supports the claim before implementing the information into your training guidelines.
Many women choose to continue their pre-pregnancy strength training program while they are pregnant, and most women may safely start strength training during their pregnancy as long as they are cleared for exercise by their healthcare provider. When developing a pregnant woman’s fitness program, you should take into account her current level of fitness and strength and pay close attention to how she feels during and after exercise. The key to maintaining a safe and effective routine is through consistent modification of the exercises for comfort as pregnancy progresses.
Strength training is an essential prenatal fitness component, providing the muscle power needed to compensate for posture adjustments and weight gain that occurs with pregnancy. Women who continue or even start a strength training routine during pregnancy can help prepare her body for all the lifting done with a new baby and reduce the risk of low back pain. Strength training has not been shown to pose any harm to either the fetus or the mother as long as these general guidelines are followed:
As always, all pregnant women should check with her healthcare provider before starting or continuing an exercise program during pregnancy.
Catherine Cram, MS started her company, Prenatal and Postpartum Fitness Consulting, in order to provide current, evidence- based guidelines maternal fitness guidelines to health and fitness professionals. She was a contributing author for the textbook, “Women’s Health in Physical Therapy” and co-authored the revision of “Exercising Through Your Pregnancy” with Dr. James Clapp. Her company offers the certification course, “Prenatal and Postpartum Exercise Design” which provides continuing education credits for over 30 health and fitness organization, including ACSM, ACE, ICEA, and Lamaze.

In 2009, 438,000 hip and 686,000 knee arthroplasties were performed in the United States, but a 2019 study projected the numbers for 2025 and 2030 to be…

Short answer: Absolutely.
Focused attention has the power to improve your health, mood and cognition. When it comes to moving steadier, research shows that practicing mindfulness while walking can improve balance in older adults. This is a simple practice that anyone can do to move more freely and live more fully with more confidence.

Being mindful means to simply focus on the present moment. Its roots stem from ancient eastern and Buddhist philosophy. It includes being aware of your thoughts, feelings, sensations and the surrounding environment through a gentle, nurturing lens. This way you can tune into what you are sensing in the present moment rather than living in and rehashing the past or projecting into the future.
Do a PubMed search on “mindfulness and health” and 14,955 studies pop up in the National Library of Medicine! These research studies show there are numerous well-being benefits that can help people of any age with any health condition including:
One foundational way that mindfulness and meditation improve health is by calming your nervous system. Moving out of the sympathetic stress response and into the parasympathetic relaxation response is where health happens. It’s where the body can rest, digest, heal and repair itself.
Constantly living in “stress mode” where you always feel overwhelmed, fearful or tense puts your body into a chronic state of inflammation that damages cells, tissues and organs. This damage accumulates and can lead to impaired bodily systems from your nervous system, respiratory, cardiovascular, musculoskeletal, and immune system. This can result in inflammaging where the body is under constant stress and strain and breaks down more than it can repair itself. It is a major reason for the age-related decline in physical and cognitive function that makes it more difficult to move and think smoothly and easily.
It’s well-accepted that practicing Tai Chi improves ankle proprioception and balance. Now studies are showing that walking meditation can do the same for elderly women and older adults with history of falling (1, 2). Walking meditation has even been shown to improve ankle proprioception and balance performance in people with chronic ankle instability! (3)
Walking meditation is a mindfulness practice where you walk slowly while focusing your attention on your leg and foot movements (2). Researchers saw improved ankle proprioception and balance improvements with older adults being able to stand on one leg for a longer time as well as increased neuromuscular control. When focusing your attention on your movement, researchers think that this improves the brain processes related to body awareness and balance adjustments (1).
Stronger neural and muscular connections mean you can be faster to sense and respond to your everyday environment, as well as recover from the loss of balance to effectively prevent a life changing injury or fall.
For the happiest, healthiest and safest holiday season, before engaging in activity, focus on “BEAM” to relieve stress, boost mood, build a sharper brain, taller posture and better balance. BEAM is an acronym that stands for Breathe, Elongate, Align and Move Mindfully.
You can imagine being as long, strong and sturdy as a “beam.” Another meaning of “beam” is to be happy, smiling and radiating a line of bright light or energy. Visualizations can enhance physical and emotional well-being and help bring your attention into the present moment.
Breathe: take 3-4 deep breaths into the front, back and sides of your belly, up into your ribs and then chest; exhale in the opposite direction from your chest, ribs and then squeeze your belly button towards your spine.
Elongate: lengthen your spine on each inhalation lifting from the crown of your head
Align your body: feel light with body parts lined up; ears over shoulders, shoulders over hips, hips over knees and ankles. Practice standing with feet hip distance apart, toes pointing forward and knees softly bending over your second and third toes; pelvis is in neutral, your sternum lifts up and out with ribs aligned over pelvis, shoulders are back and down away from the ears, line up ears over shoulders that are over hips, knees and ankles.
Move Mindfully: think about where you are and what you are about to do; whether you are cooking, cleaning, going up or down stairs or walking inside or outside focus on your leg and foot movements
Practice BEAMing throughout your day so you can move mindfully and enjoy feeling sharper, steadier, lighter and more confident with each step you take throughout the holiday season.
Millions of people over age 65 looking for guidance from fitness professionals who are knowledgeable in exercise, nutrition and lifestyle principles that can help them improve functional mobility, while also preventing and managing chronic conditions to live their highest quality of life. The Geriatric Fitness and Lifestyle Specialist online certificate course will give you insights, strategies and tools to be a successful professional in this rapidly growing market. Learn how to be a valued part of clients’ continuum of care, working with the medical team to improve functional outcomes and positively impact people’s lives.

Cate Reade, MS, RD is a Registered Dietitian and Exercise Physiologist on a mission to improve functional mobility and health span utilizing the power of lifestyle medicine. She has been teaching, writing and prescribing healthy eating and exercise programs for over 25 years. Today, as CEO of Resistance Dynamics and inventor of the MoveMor™ Mobility Trainer, she develops exercise products and programs that target joint flexibility, strength and balance deficits to help older adults fall less and live more.
References