Inflammaging: The Link Between Sarcopenia and Cognitive Decline
Awareness is the first step to making changes to live healthier, stronger, and longer. Older adults love to learn, and sharing life-saving information empowers them.
If you ask an older adult client, “What is inflammaging?”, they usually won’t know; yet inflammaging is a key concept to understand because it contributes to the decline of the body and brain, threatening functional independence, and increasing the risk of a devastating fall.










 The above is a standard sentence during my PAC Profile assessments and it carries with it powerful proactivity. I just also serendipitously learned that “proactivity” is a real, bona-fide word. When we teach movement, it makes sense to demonstrate first. Explaining to anybody a physical activity they’ve never performed, or performed with questionable technique, will skew towards wheels-fall-off territory early. Proactive practices give us and our athletes more opportunity sooner, and reduce the need to backtrack.
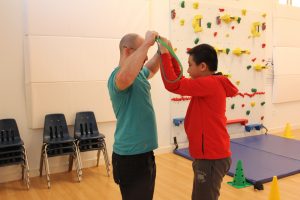
The above is a standard sentence during my PAC Profile assessments and it carries with it powerful proactivity. I just also serendipitously learned that “proactivity” is a real, bona-fide word. When we teach movement, it makes sense to demonstrate first. Explaining to anybody a physical activity they’ve never performed, or performed with questionable technique, will skew towards wheels-fall-off territory early. Proactive practices give us and our athletes more opportunity sooner, and reduce the need to backtrack. Efficient and effective coaching enables us to determine how best the athlete will learn a particular exercise. While it’s tempting to classify our athletes as “more visual” or “more kinesthetic” learners I’ve found that it is far better to approach this from an exercise-by-exercise basis. Some of my athletes need physical prompting through the end range of an overhead press but can “get” a band row when I demonstrate pulling my arms back while standing parallel to them.
Efficient and effective coaching enables us to determine how best the athlete will learn a particular exercise. While it’s tempting to classify our athletes as “more visual” or “more kinesthetic” learners I’ve found that it is far better to approach this from an exercise-by-exercise basis. Some of my athletes need physical prompting through the end range of an overhead press but can “get” a band row when I demonstrate pulling my arms back while standing parallel to them.