Pisa Syndrome and Parkinson’s Disease
If you work with people living with Parkinson’s disease then you’ve learned that every PD “fighter” experiences their own unique combinations of symptoms. Someone might have a tremor, hypophonia, and cognitive issues, while another struggles with rigidity, balance, vestibular issues and Pisa Syndrome. Wait. What is Pisa Syndrome?
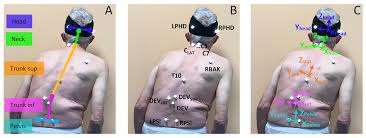
Pisa Syndrome, also known as Pleurothotonus, affects the spine and is defined as a lateral bending of the trunk with a tendency to lean to one side. Pisa causes changes in the spine such as narrowing of the central spinal canal through which the spinal cord travels leading to stenosis, poor posture and instability.
It is common for Pisa and Scoliosis to be considered the same problem. However, they are not. A person living with Pisa will “list” to one side, while a person living with Scoliosis will have an S or C curvature to their spine and rotation but not necessarily a lateral bend.

What Causes Pisa Syndrome?
It is likely that Pisa is multifactorial, meaning many factors may influence the development of and severity of Pisa Syndrome. We think there is a central (brain and spinal cord) component to Pisa Syndrome involving basal ganglia dysfunction (dystonia and rigidity), abnormal sensory integration, and/or cognitive dysfunctions affecting perception and postural control. Additionally, there is dysfunction with the Peripheral mechanisms consisting of alterations of the musculoskeletal system (myopathy, soft tissue changes).
There is some conjecture that due to medication changes or the increase of the dose of dopaminergic medications, the likelihood of Pisa onset becomes higher. Do not make medication changes without discussing with your care team. Other scientists think that as basal ganglia dysfunction increases, so do the chances of Pisa (Tinazzi et al., 2019; Artusi et al., 2019).
Is Pisa Syndrome Neurological AND Bone-related?
Yes! Because Pisa is associated with basal ganglia and sensorimotor dysfunction, there is a high likelihood of the onset of Pisa with various movement disorders, such as idiopathic Parkinson’s (80% of the Parkinson’s population) and atypical Parkinson’s syndromes (20% of the Parkinson’s population), such as Multiple Systems Atrophy, dementia with Lewy Bodies, Progressive Supranuclear Palsy (Castrioto et al, 2014; Barone et al., 2016).
Although Pisa syndrome is usually classified as a neuromuscular disorder, the spine is greatly affected due to favoring one side, leading to postural abnormalities. This can affect not only muscular health and movement, but also bone health. Bad posture, overcompensation for balance to one side, issues such as falling, and increased risk for osteoporosis may be more likely to occur in those individuals with Pisa, resulting in the likelihood of bone fractures and overall decreased bone health (Barone et al., 2016).
Medication Awareness
Moving on, let’s investigate how medication may affect Pisa Syndrome. Although there are studies correlating the use of dopaminergic drugs, there is no longitudinal or concrete evidence stating that medication causes Pisa syndrome (Castrioto et al., 2014; Barone et al., 2016; Tinazzi et al., 2016). However, it is known that incorrect dosages, either too high OR too low, can affect the onset of this disorder (Castrioto et al., 2014; Tinazzi et al., 2016). Therefore, it is imperative that providers assess the correct dosage, and that medication is taken consistently to lessen chances of this syndrome.
Some medications that may contribute to the onset of Pisa syndrome include dopaminergic medications such as carbidopa-levodopa (Sinemet or generic), dopamine agonists such as ropinirole, or anticholinesterases such as donepezil. This may sound scary, but it is important to note that Pisa can be treated by adjusting PD medications, so make sure to advise fighters to check in with their doctor if they are experiencing Pisa symptoms.
The Effect of Pisa Syndrome On Parkinson’s Disease
Now that we’ve looked at Pisa from a scientific perspective, let’s address how Pisa Syndrome affects activities of daily living and Parkinson’s Disease.
As mentioned earlier, Pisa Syndrome essentially causes changes in the spine which leads to poor posture and instability and causes the following:
- The head may droop.
- The neck moves forward rather than remaining in alignment with the spine.
- The shoulders round causing a forward slump that affects the amount of space for your internal organs.
- Breathing becomes shallow and/or more labored.
- Movement through the hips and spine decreases which affects gait length and increases risk of falls.
The above postural changes can impact one in the following ways:
- Neck/Jaw pain and headaches due to muscle tightness
- Loss of sleep
- Digestion disruption due to organs being compressed
- Depression
- Poor circulation
- Constricted nerves
- Foot pain due to misalignment
- High blood pressure
Sensory Components of Pisa
Here we see how the three balance systems are impaired:
- Vision: Impaired perception of vertical (vertical can deviate either towards or away from the side the body tilts).
- Proprioceptive: Unbalanced proprioceptive feedback (body awareness in relation to space and time).
- Vestibular: Unilateral or possible bilateral vestibular hypofunction.
Treatment for Pisa Syndrome
Let’s consider some of the activities a person does during the day-to-day – walking, bathing, dressing, cleaning, laundry, caring for children/spouse/pets, cooking, driving, social events.
We don’t have any concrete data on if/how Pisa affects Parkinson’s severity, but we can see from the above how it may affect Parkinson’s symptoms. So, how can we treat Pisa? Let’s have a look.
1. Medication – Advise fighters/care partners to speak to their physician. Encourage them to review their medications with their physician to see if changes in dosage or type of drug may be initiating or aggravating the syndrome.
2. Reducing Fall Risk – Pisa Syndrome can increase the risk of falls secondary to a lateral trunk lean which results in a change in the center of gravity and inadequate trunk control. As such, one should seek a comprehensive evaluation aimed at eliminating risk factors for falls, improving postural awareness, strength/mobility training, and/or offering effective preventive measures to reduce fall risk. This can be performed by a multidisciplinary team consisting of a physician, personal trainer, and physical therapist.
Additionally, and importantly, a major goal of physical therapy is improving midline awareness and making sure that their curvature does not worsen.
3. Exercise – Addressing your fighters core through exercises that involve vertical and lateral challenges provide the most benefit. While we cannot change the shape of the spine, we can strengthen the muscles that support the core!
- Rows
- T’s
- Front Lateral Pulldown
- Shrugs (standing upright)
- Modified Cobra (hands on the kitchen counter or ballet barre to protect those
- with Osteoporosis and Osteopenia)
- Tube rotation exercises
- Isometric tube exercises
- Stretching to maintain spinal mobility
- Trunk alignment and midline orientation exercises
- Physical Therapist to assess for somatosensory integration deficits which
- Vision
- Vestibular
- Proprioceptive
*Below, you’ll find a video demonstration to learn how to properly perform these exercises. Bridges For Parkinson’s includes these exercises in the warm-up and strength portion of our routines each week.
Note: Some may need individualized physical therapy to provide postural exercises, reduce lumbar pain, and provide preventative exercises.
In closing, Pisa Syndrome is unique in that it develops over time in conjunction with a movement disorder. The strength of a person’s physical structure depends on having the knowledge to identify possible bone issues such as Pisa Syndrome, properly addressing the issue with corrective exercises and a team that provides support and encouragement.
Bridges For Parkinson’s is focused on helping Parkinson’s fighters, care partners and fitness professionals develop a sense of awareness and provide corrective exercise therapy for those dealing with Pisa Syndrome along with preventative exercises to support a strong, vertical spine!
Parkinson’s Disease is a journey and Bridges For Parkinson’s – Rock Steady Boxing Music City and Franklin wants to support you and your Parkinson’s “fighters” on the journey. As a MedFit author and Parkinson’s Fitness Professional, I am here to help.
Together, we fight back stronger!
Fit Pros: You Can Improve the Lives of Those Living with Parkinson’s
Enroll in Colleen’s 12-hour online course, Parkinson’s Disease Fitness Specialist. The course brings the research, medical and fitness fields together so that fitness professionals gain a comprehensive understanding of Parkinson’s disease, and learn how to work with those who have it.

Written by
- Colleen Bridges, M. Ed., NSCA-CPT, Parkinson’s Disease Fitness Specialist, Founder of Bridges For Parkinson’s
- Renee Rouleau- PhD candidate, Jacobs School of Biomedical Sciences, University at Buffalo
- Betsy Lerner, MA English & African American Lit., ISSA-CPT, Parkinson’s Disease Specialist and Rock Steady Boxing Certified
- Megan Kelly, PT, DPT, LSVT Big and Parkinson’s Wellness Recovery Certified
- Cindy Nyquist, LPTA, ATC, Rock Steady Boxing Certified
References
- Huh, Y. E., Kim, K., Chung, W.-H., Youn, J., Kim, S., & Cho, J. W. (2018). Pisa syndrome in parkinson’s disease: Pathogenic roles of verticality perception deficits. Scientific Reports, 8(1). https://doi.org/10.1038/s41598-018-20129-2
- Huh, Y. E., Seo, D.-W., Kim, K., Chung, W.-H., Kim, S., & Cho, J. W. (2022). Factors contributing to the severity and laterality of Pisa syndrome in parkinson’s disease. Frontiers in Aging Neuroscience, 13. https://doi.org/10.3389/fnagi.2021.716990
- Di Lazzaro, G., Schirinzi, T., Giambrone, M. P., Di Mauro, R., Palmieri, M. G., Rocchi, C., Tinazzi, M., Mercuri, N. B., Di Girolamo, S., & Pisani, A. (2018). Pisa syndrome in parkinson’s disease: Evidence for bilateral vestibulospinal dysfunction. Parkinson’s Disease, 2018, 1–6. https://doi.org/10.1155/2018/8673486
- Artusi CA, Montanaro E, Tuttobene S, Romagnolo A, Zibetti M and Lopiano L (2019) Pisa Syndrome in Parkinson’s Disease Is Associated With Specific Cognitive Alterations. Front. Neurol. 10:577. doi: 10.3389/fneur.2019.00577
- Barone P, Santangelo G, Amboni M, Pellecchia MT, Vitale C. Pisa syndrome in Parkinson’s disease and parkinsonism: clinical features, pathophysiology, and treatment. Lancet Neurol. 2016 Sep;15(10):1063-74. doi: 10.1016/S1474-4422(16)30173-9. Epub 2016 Aug 8. PMID: 27571158
- Castrioto, A., Piscicelli, C., Pérennou, D., Krack, P. and Debû, B. (2014), The pathogenesis of Pisa syndrome in Parkinson’s disease. Mov Disord., 29: 1100-1107. https://doi.org/10.1002/mds.25925
- Huh YE, Seo D-W, Kim K, Chung W-H, Kim S and Cho JW (2022) Factors Contributing to the Severity and Laterality of Pisa Syndrome in Parkinson’s Disease. Front. Aging Neurosci. 13:716990. doi: 10.3389/fnagi.2021.716990
- Tinazzi, M., Geroin, C., Gandolfi, M., Smania, N., Tamburin, S., Morgante, F. and Fasano, A. (2016), Pisa syndrome in Parkinson’s disease: An integrated approach from pathophysiology to management. Mov Disord., 31: 1785-1795. https://doi.org/10.1002/mds.26829
- Tinazzi, M., Gandolfi, M., Ceravolo, R., Capecci, M., Andrenelli, E., Ceravolo, M.G., Bonanni, L., Onofrj, M., Vitale, M., Catalan, M., Polverino, P., Bertolotti, C., Mazzucchi, S., Giannoni, S., Smania, N., Tamburin, S., Vacca, L., Stocchi, F., Radicati, F.G., Artusi, C.A., Zibetti, M., Lopiano, L., Fasano, A. and Geroin, C. (2019), Postural Abnormalities in Parkinson’s Disease: An Epidemiological and Clinical Multicenter Study. Mov Disord Clin Pract, 6: 576-585. https://doi.org/10.1002/mdc3.12810