The Naturopathic Chef: Asparagus Quinoa with Lemony Dressing
Adding vegetables to whole grains always makes for a hearty side dish that can easily double as an entree. This is an easy way to start the transition to a plant-based diet, too. It’s one of my personal go-to’s when I’m tight on time, or when I feel like something a little lighter in the evening. You know spring has sprung when you see asparagus! As we move closer to summer, serve this chilled, over tender lettuce.
Asparagus Flavored Quinoa
- 1/2 lb Asparagus
- 1 1/2 cups Vegetable Broth
- 1 cup Quinoa, toasted
- Cheesecloth or light kitchen towel
Dressing
- 1 tsp Lemon zest
- 1 tbls Lemon juice
- 1 tsp Dijon mustard
- 2 tsps Olive oil
- Salt and Pepper to taste (I like white pepper for this recipe)
- 2 Tbls Pine nuts
 Wash and dry asparagus. Nature will tell you where to remove the fibrous part of the spear. By holding the spear, one end in each hand, begin to bend the asparagus into an arch. The spear will snap at just the right spot; no guesswork involved. Do this until all spears are free of these inedible ends.
Wash and dry asparagus. Nature will tell you where to remove the fibrous part of the spear. By holding the spear, one end in each hand, begin to bend the asparagus into an arch. The spear will snap at just the right spot; no guesswork involved. Do this until all spears are free of these inedible ends.
Chefs, you know we don’t throw anything away! Let’s infuse our broth with delicious and nutritious asparagus flavor. Pour broth into a medium saucepan. Add the fibrous ends, and bring to a boil. While infusing your broth, cut the remaining asparagus into 1-inch pieces. Set aside.
Rinse quinoa thoroughly. Once you can smell the aroma of asparagus, remove ends from broth with a slotted spoon and discard. Whisk Quinoa and Asparagus pieces into the infused broth. Bring back to a boil. Reduce heat, cook uncovered 15 minutes. Turn off heat, drape towel over pan, cover with tight-fitting lid. This technique keeps condensation from falling onto our cooked grains and making them mushy. Allow to rest for 5 minutes.
In a small bowl, whisk together lemon zest through salt and pepper. Warm a serving bowl and fluff quinoa with a fork. Gently pour finished quinoa into serving bowl. Drizzle with dressing and fluff lightly. Sprinkle with pine nuts and some beautiful asparagus tips.
Phyto Facts
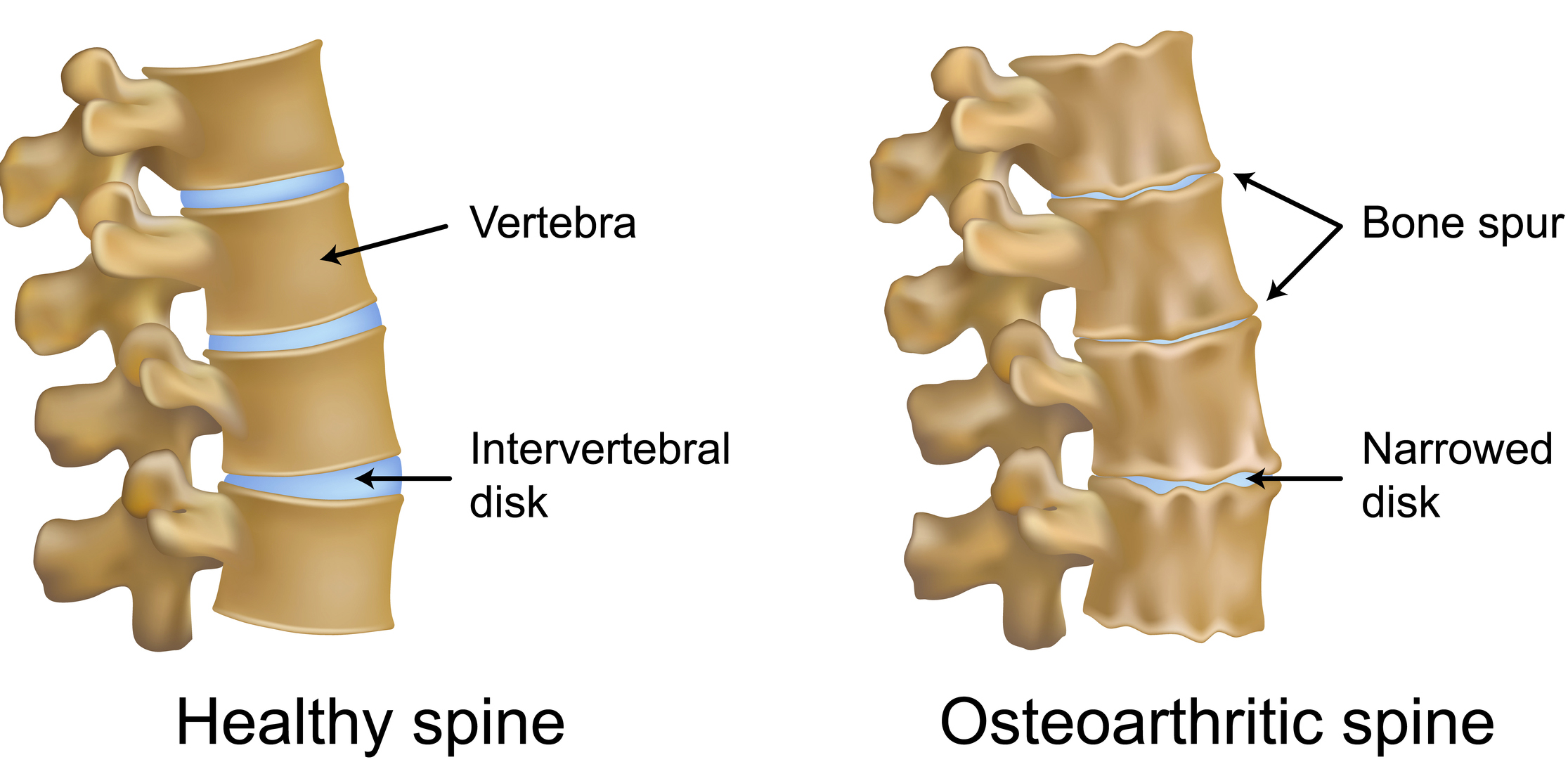
To date, asparagus is our greatest hope in finding the cure for ALS, Amyotrophic Lateral Sclerosis, or Lou Gehrig’s disease. The phytonutrient, Sarsasapogenin, prevents motor-neuron cell death. It’s also housed in inulin. A fibrous carbohydrate, it lowers blood sugar due to the small intestines inability to break it down. This allows the nutrients to make their way to the large intestines, where it feeds good bacteria, making it a very effective probiotic. This combination of natural activity makes it very effective in treating degenerative disease, i.e., ALS, Type 2 Diabetes, and Crohn’s Disease.
The presence of four other phytonutrients, known as anti-inflammatory powerhouses: Kaempferol, Quercitin, Rutin, and Isorhamnetin, give it major cancer-killing abilities. I have used asparagus, with great success, in the treatment and complete eradication of melanoma. Being very high in minerals, and antioxidants like Vitamins C and E, it is, generally speaking, a great way to prevent nutrient deficiency overall.
Asparagus also contains a good amount of Glutathione — a combination of three amino acids combined into one molecule. This, many researchers believe, will eventually be the cure for Parkinson’s disease. Rich in soluble and insoluble fiber, asparagus not only breeds good bacteria in the digestive/intestinal tracts, it’s also a vegan’s best friend, as it is one of the richest sources of veggie protein.
The odor when one urinates after eating asparagus: sulfuric compounds. This group of phytonutrients prevents hormone and digestive based cancers better than any other group of phytos. This odor lets you know you are digesting the nutrients effectively. This is about the only time stinky pee is a sign of good health! So, enjoy… the asparagus, not the odor.
Get more great recipes from Tina Martini — her book, Delicious Medicine: The Healing Power of Food is available to purchase on Amazon. More than a cookbook, combining 20+ years of experience, along with her love of coaching, cooking and teaching, Tina offers unexpected insights into the history and healing power of clean eating, along with recipes to help reduce your risk of disease and improve overall wellness so you can enjoy life!
Affectionately referred to as The Walking Encyclopedia of Human Wellness, Fitness Coach, Strength Competitor and Powerlifting pioneer, Tina “The Medicine Chef” Martini is an internationally recognized Naturopathic Chef and star of the cooking show, Tina’s Ageless Kitchen. Tina’s cooking and lifestyle show has reached millions of food and fitness lovers all over the globe. Over the last 30 years, Tina has assisted celebrities, gold-medal athletes and over-scheduled executives naturally achieve radiant health using The Pyramid of Power: balancing Healthy Nutrition and the healing power of food, with Active Fitness and Body Alignment techniques. Working with those who have late-stage cancer, advanced diabetes, cardiovascular and other illnesses, Tina’s clients are astounded at the ease and speed with which they are able to restore their radiant health. Tina believes that maintaining balance in our diet, physical activity, and in our work and spiritual life is the key to our good health, happiness and overall well being. Visit her website, themedicinechef.com








 Have you ever wondered why a particular diet, workout routine or cleanse offers remarkable results for some people, but not others?
Have you ever wondered why a particular diet, workout routine or cleanse offers remarkable results for some people, but not others?