5 Simple Exercises To Help Symptoms Of Rheumatoid Arthritis
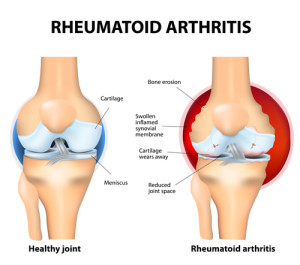 When left unchecked, rheumatoid arthritis can be majorly debilitating and cause real and continued pain. However, if you’re willing to do the research and put in the work, you can do certain exercises which can majorly reduce the symptoms, improve your overall mood and actually make you that much physically healthier, generally speaking, which can only be a good thing. The real question then is, what sort of exercises ought you be doing to try and achieve this. Well, let’s take a look at five ways to help improve those symptoms.
When left unchecked, rheumatoid arthritis can be majorly debilitating and cause real and continued pain. However, if you’re willing to do the research and put in the work, you can do certain exercises which can majorly reduce the symptoms, improve your overall mood and actually make you that much physically healthier, generally speaking, which can only be a good thing. The real question then is, what sort of exercises ought you be doing to try and achieve this. Well, let’s take a look at five ways to help improve those symptoms.
Start Stretching
Stretching is actually something which we all ought to do and can be a great way to start anyone’s day. Daily stretching reinforces a healthy sense in which the muscles are able to become increasingly limber and flexible across time. Stretching is a personal thing, and it will depend a bit on where most of your arthritis pain is concentrated. When you stretch you want to go slowly and thoroughly. Warm up for a few minutes and then stretch each of the muscles you want slowly, pushing yourself further in tiny intervals. To guarantee success, track down a physical therapist with an understanding of rheumatoid arthritis.
A Focus On The Hands
“It’s all too common that rheumatoid arthritis has an adverse and painful effect on the hands, meaning this is an area which ought to be focused on in terms of exercises that can be done”, advises Charles Tevesham, health writer at LastMinuteWriting and Writinity. There are only a limited number of ways in which one can move one’s hands, so you ought to do your best to try and explore the full range of stretches available. Using a stress ball and a small roller can help to achieve this as well.
Go For Walks
Sometimes when you are in pain, having to get up and go on a walk can be the last thing that you want to do. But, it’s hugely beneficial. The act of walking involves so many of the different muscle groups and makes it so easy to do something that will be beneficial for your arthritis. It is also a great way to boost your mood, since it is exercise and involves being outdoors. Make sure you drink water and try to slowly increase your speed across the duration of your walk.
Water-Based Exercises

Completing exercises, stretches and other forms of aerobics in a pool is a wonderfully forgiving way of going about your pain reduction routine. Being in water helps to reduce the impact of your body weight so it makes it very easy to do exercises without fearing that you are going to injure yourself. Furthermore, the act of swimming is actually a really good exercise that involves using all o the muscle types in your body in a way which is actually deeply therapeutic and relaxing. If the water is warm, that’s an even better way to soothe pain.
Get On Your Bike
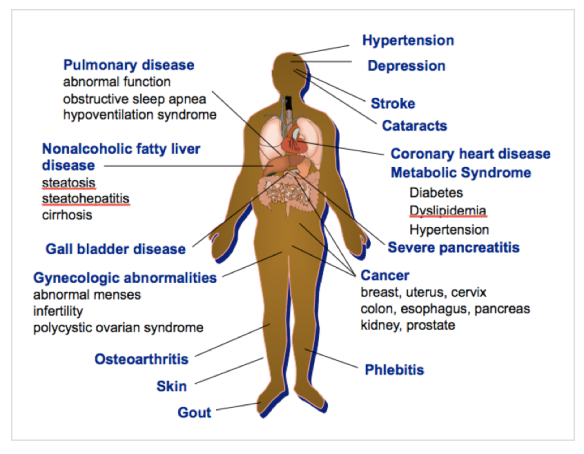
Cycling is another good exercise option. “Cycling is definitely one of the more strenuous options available to you, but it’s one that will really help ensure that the increase in the risk of cardiovascular problems that rheumatoid arthritis involves, doesn’t get the better of you”, says Mary Simmons, health blogger at DraftBeyond and ResearchPapersUK. You ought to make sure that you have stretched thoroughly before you get onto a bike as the intense locational nature of the workout, in other words the amount of pressure it puts your leg muscles under, can cause you an injury. That said, it’s an incredibly good way to exercise the muscles in the lower half of your body and has long term benefits to flexibility and pain reduction.
Conclusion
Overall, stretching and various other exercises are actually vitally important to giving yourself the best chance of avoiding unnecessary and difficult to deal with pain. Rheumatoid arthritis is never going to be pleasant, but if you really commit to a routine of exercise you can be sure that the way you feel, physically and mentally, is going to improve and that steps towards managing the symptoms will be moved through quickly.
Harry Conley is a content editor at LuckyAssignments and GumEssays. He develops training procedures and manages the workflow to give writers supplemental support instruction. A man of many interests, Harry also works in providing supplementary materials and instructional support for contributors.
References
Charles Tevesham, health writer, LastMinuteWriting and Writinity.
Mary Simmons, health blogger, DraftBeyond and ResearchPapersUK



 Those living with arthritis can live well and have a good quality of life by employing lifestyle interventions as medicine, in conjunction with, prevention, joint protection, weight management, physical activity, wise food choices, stress management and a good medical regimen. By combining all these necessary recommendations into a personalized Wellness Strategy and Plan, a coach can assist an arthritis patient in organizing what is important for them to live life well. The Wellness Plan then becomes a map by which to navigate toward managing and maximizing the patient’s best life possible.
Those living with arthritis can live well and have a good quality of life by employing lifestyle interventions as medicine, in conjunction with, prevention, joint protection, weight management, physical activity, wise food choices, stress management and a good medical regimen. By combining all these necessary recommendations into a personalized Wellness Strategy and Plan, a coach can assist an arthritis patient in organizing what is important for them to live life well. The Wellness Plan then becomes a map by which to navigate toward managing and maximizing the patient’s best life possible.
 these gaps between the medical team and patient by following up with patients and guiding a patient-centered approach, asking about needs and addressing obstacles, addressing health literacy, cultural issues and social-class barriers.
these gaps between the medical team and patient by following up with patients and guiding a patient-centered approach, asking about needs and addressing obstacles, addressing health literacy, cultural issues and social-class barriers.
 The most important factor in the safety and efficacy of the exercise program is the initial assessment. At the very least this should include a comprehensive postural assessment as well as shoulder range of motion measurements taken with a goniometer. The well-trained fitness professional will be able to deduce, from the results, which muscles need to be stretched and which need to be strengthened. By selecting the wrong combinations of exercises, the results may not only be undesirable, they may in fact be detrimental. For example, if a client presents with moderate to severe upper-crossed syndrome, performing any kind of “pushing” exercise that would involve the chest muscles (chest press), could make the syndrome even more pronounced by causing the pectoral muscles to tighten and contract. Instead, the goal need to be on stretching the chest wall and strengthening the opposing muscles in the back; particularly the scapular stabilizers.
The most important factor in the safety and efficacy of the exercise program is the initial assessment. At the very least this should include a comprehensive postural assessment as well as shoulder range of motion measurements taken with a goniometer. The well-trained fitness professional will be able to deduce, from the results, which muscles need to be stretched and which need to be strengthened. By selecting the wrong combinations of exercises, the results may not only be undesirable, they may in fact be detrimental. For example, if a client presents with moderate to severe upper-crossed syndrome, performing any kind of “pushing” exercise that would involve the chest muscles (chest press), could make the syndrome even more pronounced by causing the pectoral muscles to tighten and contract. Instead, the goal need to be on stretching the chest wall and strengthening the opposing muscles in the back; particularly the scapular stabilizers. Following the warm-up and lymph drainage exercises, the exercise specialist should determine what the areas of “need” are for the client. Remember to begin with stretching and range of motion exercises until they have close to “normal” range of motion. At that point the goal becomes strength training and choosing exercises that will strengthen the weaker muscles and stretch the tight and shortened muscles. Weight/resistance should also be very gradually increased and attention paid to any potential swelling of the extremity. Typically I chose exercises that will stretch the chest (chest fly, corner or door stretch, assisted stretching) and will strengthen the back (low/high rows, reverse flies, lat pulldown). They often [present with winged scapula following a node dissection. If this is the case, I will incorporate exercises that will strengthen the serratus anterior. If they have undergone an abdominal TRAM procedure, core work will be of the greatest importance in preventing, or minimizing, low back pain.
Following the warm-up and lymph drainage exercises, the exercise specialist should determine what the areas of “need” are for the client. Remember to begin with stretching and range of motion exercises until they have close to “normal” range of motion. At that point the goal becomes strength training and choosing exercises that will strengthen the weaker muscles and stretch the tight and shortened muscles. Weight/resistance should also be very gradually increased and attention paid to any potential swelling of the extremity. Typically I chose exercises that will stretch the chest (chest fly, corner or door stretch, assisted stretching) and will strengthen the back (low/high rows, reverse flies, lat pulldown). They often [present with winged scapula following a node dissection. If this is the case, I will incorporate exercises that will strengthen the serratus anterior. If they have undergone an abdominal TRAM procedure, core work will be of the greatest importance in preventing, or minimizing, low back pain.

 Another benefit of exercise for stroke survivors is prevention of recurrent stroke or heart attack, which occurs frequently in people who have had a stroke.(3) Reducing risk factors can decrease the incidence of recurrent strokes and coronary events. An aerobic conditioning program can enhance glucose regulation and promote decreases in body weight and fat stores, blood pressure, C-reactive protein, and levels of total blood cholesterol, serum triglycerides, and low-density lipoprotein cholesterol.(4) Exercise also increases high-density lipoprotein cholesterol and improves blood rheology, hemostatic variables, and coronary endothelial function.(5)
Another benefit of exercise for stroke survivors is prevention of recurrent stroke or heart attack, which occurs frequently in people who have had a stroke.(3) Reducing risk factors can decrease the incidence of recurrent strokes and coronary events. An aerobic conditioning program can enhance glucose regulation and promote decreases in body weight and fat stores, blood pressure, C-reactive protein, and levels of total blood cholesterol, serum triglycerides, and low-density lipoprotein cholesterol.(4) Exercise also increases high-density lipoprotein cholesterol and improves blood rheology, hemostatic variables, and coronary endothelial function.(5)




 In the
In the  Focusing on a few exercises also gives our athletes the opportunity to learn the name and typical order in which the exercises can be performed. Whereas our warm-up/mobility section nearly always features hurdle steps, overhead resistance band walks, bear walks/crawls, and medicine ball throws (push, overhead, and scoop), our strength/focus section includes squats, presses, pulls, farmers walks, and heavy carries.
Focusing on a few exercises also gives our athletes the opportunity to learn the name and typical order in which the exercises can be performed. Whereas our warm-up/mobility section nearly always features hurdle steps, overhead resistance band walks, bear walks/crawls, and medicine ball throws (push, overhead, and scoop), our strength/focus section includes squats, presses, pulls, farmers walks, and heavy carries.
 Apigenin
Apigenin