Meditation for Fibromyalgia
Fibromyalgia is a condition where there is muscle pain, fatigue, and tender spots on the body. While there is no cure for this condition meditation may help you to cope with the symptoms. There are many benefits of meditation for Fibromyalgia including: decreased stress, feeling more at ease, decreased blood pressure and heart rate, decreased anxiety, increased energy and pain tolerance.






 Sometimes, being active can actually make it more challenging for you to manage your blood glucose (“blood sugar”) levels, unless you learn more about its effects. I have always known at some level that exercise generally did good things for my blood glucose, even before I had my first blood glucose meter (after going 18 years without access to one). How could I tell without a blood glucose meter?
Sometimes, being active can actually make it more challenging for you to manage your blood glucose (“blood sugar”) levels, unless you learn more about its effects. I have always known at some level that exercise generally did good things for my blood glucose, even before I had my first blood glucose meter (after going 18 years without access to one). How could I tell without a blood glucose meter? Over a longer period of time (2-3 hours), it usually comes back down, but who wants to wait that long?
Over a longer period of time (2-3 hours), it usually comes back down, but who wants to wait that long?
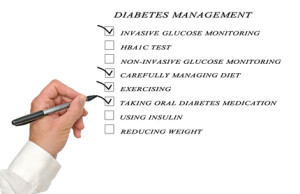 According to the New England Journal of Medicine, “Type 2 diabetes is increasingly common, primarily because of increases in the prevalence of a sedentary lifestyle and obesity. It was concluded that the reduction in the incidence of diabetes was directly associated with changes in lifestyle and that Type 2 diabetes can be prevented by changes in the lifestyles of high-risk subjects.”
According to the New England Journal of Medicine, “Type 2 diabetes is increasingly common, primarily because of increases in the prevalence of a sedentary lifestyle and obesity. It was concluded that the reduction in the incidence of diabetes was directly associated with changes in lifestyle and that Type 2 diabetes can be prevented by changes in the lifestyles of high-risk subjects.” What Can Health & Wellness Coaches Do for You?
What Can Health & Wellness Coaches Do for You?



