VO2 Max: Connecting the Dots Between Fitness Metrics and Healthcare
Cardiovascular fitness has become universally acknowledged as a major determinant of health outcomes. Yet relatively few fitness facilities help their members quantify fitness in the way that is recognized by the research and medical communities as being scientifically valid. As the fitness and medical communities become more connected and increasingly partner with one another, a common language about cardiovascular fitness should be used.



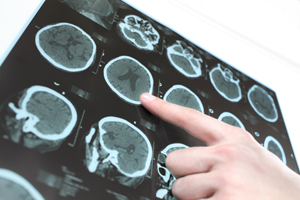
 Contrary to popular belief, neurogenesis continuously occurs in the adult brain under the right conditions such as with exercise. Substantial benefits on cognitive test performance were noted for combined physical and cognitive activity than for each activity alone. It was also noted that the physical and cognitive exercise together might interact to induce larger functional benefits. “We assume, that physical exercise increases the potential for neurogenesis and synaptogenesis while cognitive exercise guides it to induce positive plastic change” (Bamidis, 2014). To maximize cognitive improvement, combine physical exercise with cognitive challenges in a rich sensorimotor environment that includes social interaction and a heaping dose of fun.
Contrary to popular belief, neurogenesis continuously occurs in the adult brain under the right conditions such as with exercise. Substantial benefits on cognitive test performance were noted for combined physical and cognitive activity than for each activity alone. It was also noted that the physical and cognitive exercise together might interact to induce larger functional benefits. “We assume, that physical exercise increases the potential for neurogenesis and synaptogenesis while cognitive exercise guides it to induce positive plastic change” (Bamidis, 2014). To maximize cognitive improvement, combine physical exercise with cognitive challenges in a rich sensorimotor environment that includes social interaction and a heaping dose of fun.



 I am honored that she reached out to me. I am still in “ahh”, by the whole experience. Often stroke survivors and their caregivers do not find the help needed to further their recovery after physical therapy ends. Unfortunately, some survivors do not even get good physical therapy in the crucial, early stages in recovery, when it is essentially needed. She shared with me some not so good experiences she and her husband had faced, like many others I have spoken with.
I am honored that she reached out to me. I am still in “ahh”, by the whole experience. Often stroke survivors and their caregivers do not find the help needed to further their recovery after physical therapy ends. Unfortunately, some survivors do not even get good physical therapy in the crucial, early stages in recovery, when it is essentially needed. She shared with me some not so good experiences she and her husband had faced, like many others I have spoken with.