The Concept of Movement Literacy for Joint Replacement Fitness Clients
In 2009, 438,000 hip and 686,000 knee arthroplasties were performed in the United States, but a 2019 study projected the numbers for 2025 and 2030 to be…
Lost your password? Please enter your email address. You will receive a link to create a new password.

In 2009, 438,000 hip and 686,000 knee arthroplasties were performed in the United States, but a 2019 study projected the numbers for 2025 and 2030 to be…

By 2030, the demand for primary total hip arthroplasties is estimated to grow by 174% to 572,000. The demand for primary total knee arthroplasties is projected to grow by 673% to 3.48 million procedures.
Pre-surgical or prehabilitation (prehab) programs have been gaining increased popularity and show promising results in getting clients moving quicker after surgery. Prehab can be defined as an individualized physical conditioning program to improve strength, endurance, and range of motion prior to surgery.
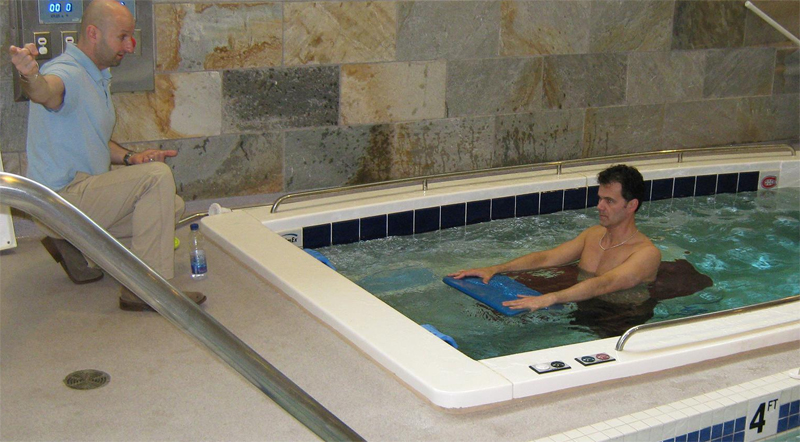
I have found in my experience that by incorporating an aquatic program six or more weeks prior to surgery can have significant benefit post-operatively.
A multicenter study performed at New England Baptist Hospital, Beth Israel Deaconess Medical Center and Harvard Medical School found that knee- and hip-replacement surgery patients who had participated in prehab for just six weeks prior to surgeries reduced the need for inpatient rehabilitation by 73 percent. This study involved water-and land-based strength training, plus aerobic and flexibility exercises.
Reduced Pain & Swelling
Clients awaiting joint replacement surgery are usually in a significant amount of pain. They may experience pain not only at the specific joint but also in corresponding joints that have compensated for improper biomechanics. Using the water’s unloading properties to reduce pain, as well as the hydrostatic pressure to help with swelling reduction, are tremendous benefits.
Restore Range of Motion (ROM)/Muscle Balance
I always tell my clients, “Motion is Lotion.” This means that the more you move correctly, the better you will feel. Gaining as much ROM prior to joint replacement is very important. I also share, “The doctor will be replacing your joint, not your ligaments, tendons or muscles. The more muscle balance we can get the better you will do post operatively.” I give the example of a worn out tire on a car. Over time the cars suspension adapts to that worn tire and pulls out of alignment. The replaced joint represents the new tire; now we have to realign the suspension so everything rides correctly.
In the water using flotation equipment on the lower extremities allows the client to gain much more ROM.
Buoyancy unloads the joint and assists the motion, but more importantly the client has control over the movement. If try to manually stretch a client, he/she is automatically guarded, no matter how much I remind them to “relax”. Moving freely in the water, the client is more likely to push their ROM than if I stretch him/her manually.
Improve Strength
Pain causes muscle inhibition and hence muscle weakening. Neuromuscular control needs to be restored prior to surgery in order to facilitate muscle recovery post-operatively. The stronger the muscles are, the faster the recovery. Strengthening exercises to help balance all muscle groups are much easier and comfortably performed in the water. Water provides an accommodating three-dimensional resistance which allows multiple muscle groups to be strengthened simultaneously.
Improve Proprioceptive Awareness & Normal Movement Patterns
Any functional movement depends on the coordination and fine tuning of the neuromuscular system. Joint degeneration affects the soft tissues that contain proprioceptors, which will cause significant reduction in the awareness of joint movement.
Proprioceptive exercises can be be started prior to surgery to stimulate the neuromuscular mechanisms and make them more responsive after surgery. The water provides a surrounding proprioceptive enriched environment to help restore neuromuscular function, including balance and proprioception.

Improve Gait
Degeneration of lower extremity joint will commonly result in a compensated gait pattern. This pattern is often continued, even after surgery, because of abnormal motor patterns. Use the water to correct gait patterns prior to surgery, which will assist with alignment, weight shift and proprioceptive input, and therefore facilitate a normal post-op gait pattern.
Client Education
Surgeons often do not tell the client what they will experience post operatively. Thus, another benefit of prehab is the opportunity to educate the client on the post-op process. Clients often compare themselves to other people who have had a similar surgery, which can lead to frustration. By educating the client and with the understanding that everyone progresses at a different rate.
In my experience, by utilizing the water for prehabilitation prior to a total joint replacement is one of the best ways to get clients moving and feeling better faster!
If you’re interested in sponsoring a Medically Based Aquatics (MBA) course at your facility, please contact Rick McAvoy at rick@rickmcavoyaquatics.com
Dr. Rick McAvoy has specialized in Aquatic Physical Therapy and Sports Performance for over 30 years and promotes aquatic fitness, rehab and training. He is the Owner of Rick McAvoy Aquatics, an Aquatic Fitness and Sports Performance Training and Consulting Company. Rick is also a published author and researcher in the field of Aquatic Therapy and Fitness as well as Sports Performance.

Proprioception refers to the conscious and unconscious perception of postural balance, muscles sense, and joint position and stability. Basically, it is your sense of where you are in time and space for movement. We have found over the years that the best way to explain proprioception to clients comes from Dr. Eric Cobb at Z-Health Performance Solutions:
“Proprioception is the body’s 3D map of itself in time and space. AKA our movement and awareness map”.
The detail and definition of this “proprioceptive map” comes from several specialized mechanoreceptors (i.e. nerve endings) in the muscles, tendons, joint capsules, fascia, and skin. As fitness trainers as we are usually taught about muscle spindles and Golgi tendon organs when we learn about flexibility training, but there is a lot more to proprioceptive input. You are affecting the proprioceptive input to the brain when you use a neoprene knee sleeve (pressure), kinesiology tape (skin stretch), heat or ice packs (temperature), TENS units (electric), etc.
Several conditions can alter proprioception, thus “clouding” the map and degrading movement sense and capability, including pain, trauma, effusion, and fatigue. A joint replacement client also likely had poor motor control of the joint in the first place that resulted in compensatory movement patterns and overuse injury over time. Complicating the matter further, although it may have been necessary, the surgery itself is an “insult” to the musculoskeletal and nervous systems.

To move a joint well, you must be able to feel the joint and surrounding tissue well. An extreme example of what can happen without the sense of touch or joint position is the story of Ian Waterman. A rare neurological illness resulted in his losing all touch and joint position sensation, effectively paralyzing him from the neck down even though the motor control area of his brain and the descending pathways to send movement information to his musculature were fine!
We can improve proprioception in several ways:
The important take away is that building a “library” of prior movement patterns is especially important for the post-medical joint replacement client. We want to get their new joint moving in multiple directions, at multiple speeds, under multiple loads.
The concept of proprioception and how to harness it is not only for joint replacement, but also for general fitness, performance, and pain clients! Begin learning a neuro-centric approach to medical fitness and how to work with joint replacement clients with our Joint Replacement Fitness Specialist online course, available through the MedFit Classroom!
Pat Marques is a Z-Health Master Trainer and NSCA-CPT specializing in training the nervous system to improve performance and get out of pain. After retiring from the Active Duty Army, Pat pursued his education and certifications in exercise science, initially working with wounded, ill, and injured soldiers. During this time that Pat discovered the power of using a neurological approach to training to get out of pain and improve fitness and performance. He currently provides exercise therapy, movement reeducation, and strength and conditioning for all levels of clients at NeuroAthlete, from chronic pain sufferers to Olympic-level and professional athletes.
References:

The gym can be a confusing place especially for individuals with health concerns. Many times, these clients are trying to navigate their workouts by themselves because they are unsure of the appropriate questions that they need to ask.
First of all, there are two different types of trainers. There are trainers who have a four year degree and certifications. These trainers are sometimes called Fitness Specialists and have had many hours of study related to a wide variety of diseases and injuries. They are used to modifying exercises and programs based on any specific condition you may have. Fitness Specialists are usually found in a medically based fitness facility affiliated with a hospital. Please note that some Fitness Specialists will specialize in a certain area. Some work with individuals with diseases and disabilities and some don’t. You can search the free MedFit Network directory to find a fitness pro in your area. In their MFN profile, you’ll find information about their condition-specific education and services.

When you finally narrow down who you might like to hire you will want to ask some questions. Please don’t be afraid to ask these questions as they will help you to decide which trainer is right for you. It is also recommended that you observe Fitness Specialists training clients.
First you want to make sure that the trainer has had experience with your condition. If not, they should be willing to research it and or speak with your doctor with your permission. There are exercise guidelines that all Fitness Specialists should follow when working with clients who have health conditions.
You will also want to ask about the trainers background. It is alright to ask about education, certifications, and years of experience. You also want to hire someone who is patient with you. This is extremely important as you figure out which exercises work best for your body. I would also like to add that you need to be patient with yourself as well. Try to relax and enjoy your training session.
Asking the questions from above help to keep you feeling confident. Exercise can seem frustrating in the beginning but you have to keep a positive mindset. In the beginning, set small goals and do the best you can during each training session.
Robyn Caruso is the Founder of The Stress Management Institute for Health and Fitness Professionals. She has 15 years of experience in medical based fitness.

One of my highest honors as a Personal Trainer has been to work alongside my clients in preparation for knee surgery and post-surgery rehabilitation. Working alongside a Physical Therapist (with the client’s permission to share information) to bring the client to a complete recovery has been a privilege and an excellent learning opportunity.
Pre and post-surgery are two very different stages, but both require the client and trainer’s knowledge, trust, and commitment. Today I will focus on the preparation for knee surgery from the perspective of a Personal Trainer.
First and foremost, the Personal Trainer must act within their scope of practice. Most nationally accredited Personal Trainer certifying agencies have clearly outlined the scope of practice that a trainer must work within.
Here are a few DO’s and DON’Ts from The American Council on Exercise (ACE) that apply to the subject of pre-knee surgery clientele.
Personal Trainers DO receive guidelines from Physicians or Physical Therapists. They DO design exercise programs, refer clients to appropriate allied health professionals or medical practitioners if needed. Trainers DO design exercise programs after a client has been released from rehab, and as trainers, we work with clients, not patients.
Personal Trainers DON’T diagnose, prescribe, treat injuries or disease, rehabilitate or work with patients.
There was a time when I would stop working with a client as they were awaiting knee surgery for fear of causing more damage. Still, after going through my own knee surgery, I realized there is much I could have done to prepare appropriately and that trainers can do for clients as they prepare for surgery to help put them in the best possible position for a full recovery.

One significant preparation step for any knee surgery, often overlooked, is upper body strength. The client will likely be on crutches or possibly a wheelchair post-surgery. When your legs are not fully functioning, you rely heavily on your upper body to move from place to place, from sitting to standing and getting to your Physical Therapy sessions. I found success doing body weight work for the upper body in preparation is very helpful and can prevent shoulder injury as the client needs to move their body from bed to crutches or crutches to toilet and the like. Lifting out of a chair and putting a large amount of body weight on the arms is exhausting and, again, can strain or injure those joints and muscles, which can put the healing process from the surgery leg on a slower rehab pace.
Body weight exercises for the client pre-surgery can be as simple as lifting and scooting themselves laterally across a bench, or maybe learning to use rail support to lift themselves out of a seated position, sitting with legs extended on a mat on the floor, lifting their hips to clear the ground to shift around. Engaging and strengthening the shoulders, biceps, triceps, and even strengthening the wrists and handgrip has excellent benefits. Encouraging core work from all six sides (Rectus abdominus – front, erector spinae – back, Obliques internal and external – right and left, diaphragm – top, and pelvic floor – bottom) to support the upper body moving the body weight is very beneficial. We also shouldn’t forget mobility and stability in the upper body to assist in recovery.
The second important step to surgery preparation is strengthening the muscles that support the knee in all directions. This will allow the client to be in the best possible condition to rehabilitate well. It may be necessary to be creative in finding ways to do this without putting weight on the knee joint. Place a high priority on mobility and strengthening in the upper leg; quadriceps, hamstrings, hips, glutes: the lower leg; gastrocnemius, soleus, tibialis, and lower leg extensor muscles.
Personal Trainers can make a difference. Stay within your scope of practice, educate yourself on knee health, and take advantage of every opportunity to collaborate with a physical therapist or medical practitioner to learn, grow, and serve your clients with the highest quality.
With knowledge, trust, and commitment, trainers can make a marked difference in the clients’ recovery.
Shannon Briggs is a multi-passionate fitness professional and educator. She brings 30 plus years of experience to a long, fulfilling career in the fitness industry. In the past 13 years at the University of Texas at Austin, Shannon has led continuing education workshops in multiple group fitness formats and topics specific to personal training; she also has written the curriculum and manuals for numerous workshops accredited by the American Council on Exercise (ACE). Shannon is currently a monthly contributor to Campus Rec Magazine for Fitness and Wellness.

The SAID Principle, Specific Adaptation to Imposed Demand, is a fundamental law of human physiology. The classic definition of this principle is “the body adapts to what it does”. A more precise, neuro-centric definition would be “the body ALWAYS adapts to EXACTLY what it does”. The takeaway is this: if you want a certain result, you must train with precision.

Joint replacements are an incredible medical innovation, but they are also incredibly traumatic events to the dermal, fascial, musculoskeletal, and nervous systems. Of specific concern for joint replacement clients are the mechanoreceptors that provide input to the brain about the joint and surrounding area through touch, pressure, stretch (skin and muscles/tendons), temperature, vibration, and movement.
Some studies have shown, depending on the type of replacement performed, joint capsule mechanoreceptors are no longer present and do not regenerate. The injuries to tissues or joints, whether acute or chronic, can result in dysfunctional proprioceptive feedback, and that is not automatically regained after joint replacement. So, we will need to train with precision to maximize and improve proprioceptive input and joint position sense.
Training with precision means taking our fitness training beyond “strengthening and stretching”. Our joint replacement clients likely got plenty of that during their physical therapy anyway. Another way to think about the SAID Principle is “use it or lose it”. If we want our joint replacement fitness clients to get the most out of their replacement, we need to program a variety of aspects:
Programming for this type of variety is very important for joint replacement clients but also for general fitness, performance, and pain clients! Begin learning a neuro-centric approach to medical fitness and how to work with joint replacement clients with our Joint Replacement Fitness Specialist online course, available through the MedFit Classroom!
Pat Marques is a Z-Health Master Trainer and NSCA-CPT specializing in training the nervous system to improve performance and get out of pain. After retiring from the Active Duty Army, Pat pursued his education and certifications in exercise science, initially working with wounded, ill, and injured soldiers. During this time that Pat discovered the power of using a neurological approach to training to get out of pain and improve fitness and performance. He currently provides exercise therapy, movement reeducation, and strength and conditioning for all levels of clients at NeuroAthlete, from chronic pain sufferers to Olympic-level and professional athletes.
References

In the U.S., approximately 300,000 people undergo a total hip replacement every year, according to Harvard Health Publishing. If you’re preparing to have this common operation, you probably have some questions about the recovery process.
The good news is that you should be able to walk within just a couple of days after the surgery. That said, it usually takes around 10-12 weeks of physical therapy before you’ll be fully ready to resume your usual daily routines.

The hip is the body’s largest joint, and it goes through natural wear-and-tear over the years. As the joint degrades, it may become necessary to replace damaged sections with artificial parts called prostheses that are typically made from metal, ceramic, or hard plastic.
Arthritis associated with aging is the most common reason why people get hip replacements. While living well with arthritis is possible in some cases, sometimes surgical intervention becomes necessary.
In addition to osteoarthritis and rheumatoid arthritis, osteonecrosis is another condition that may lead to hip joint damage. Patients who suffer from osteonecrosis don’t receive enough blood flow to the hip joint’s ball segment which leads to bone damage.
As people age, it’s normal to experience aches and pains. If the pain becomes too intense and/or persistent regardless of pain medications, it may be necessary to get a hip replacement. You may also need a hip replacement if you’re struggling to walk even with the aid of a walker or cane, if you aren’t able to climb stairs, or if the pain makes it difficult to sleep.
Everyone recovers in their own time, so you may heal faster or slower than other patients. According to WebMD, here’s what a typical recovery from hip replacement surgery looks like:
Days 1-2: In some cases, you may be able to start some light physical therapy the same day as the surgery. If you’re not ready the same day, you’ll start the following day. At this time, you’ll probably be on IV pain medications and following a liquid diet.
Days 3-4: After a few days, you should be able to walk carefully with the aid of a walker or crutches. You should be able to take pain pills instead of IV pain medications and eat solid foods.
Days 4-5: Depending on how you’re feeling and performing, you may be able to move from the hospital to your preferred place of recovery. While some patients may be able to go home at this time, others may need to stay at a rehab center for ongoing therapy.
Days 5+: After five days or so, you will need to keep performing physical therapy exercises and care for the point of incision. If you’re staying at a rehab center, they will handle everything. If you’re recovering at home, you may want to have a private duty nurse visit to ensure proper care.
Days 10-14: By the two-week mark, you should be able to stop taking pain medications. You may need to have your stitches removed if they’re not the type of stitches that dissolve on their own. You should be able to bathe or shower around this time (talk to your doctor first).
Weeks 3-6: After approximately three weeks, you should be able to handle light activities, although there may be a bit of residual soreness, especially during the evenings. You should be able to drive again after six weeks.
Weeks 10-12: By this time, you should feel fairly normal. While there may be a small amount of pain or swelling, you should be able to resume regular pre-surgery activities. You may still need to have follow-up visits with your doctor for around one year after the surgery.
If you’re considering a hip replacement, the first step is to see an orthopedic surgeon who will examine you and inquire about your medical history and any medications you might be taking. The surgeon may recommend x-rays, blood tests, and an MRI.
If the surgeon determines that a hip replacement is the correct course of action, medical professionals will guide you on the next steps you’ll need to take.

At this time, it’s important that you prepare for your post-op recovery. If you plan on recovering at home, it’s essential that you make your house habitable. For example, you won’t be able to climb stairs while recovering, so you will need to make appropriate accommodations.
Working with an educated fitness professional after your hip replacement may also help accelerate your recovery after surgery. While it may seem counterintuitive to use your hip after surgery, post-joint replacement exercise can actually aid postoperative recovery by rebuilding the strength of tendons, muscles, and ligaments around your hip joint. By working with a physical therapy or fitness professional, you also help:
Because recovering from a hip replacement usually requires professional assistance, many patients also choose to book a stay at a dedicated treatment facility for the first 48-hours to week after their procedure. This allows them to recover surrounded by healthcare professionals who can keep them comfortable while also providing patient-specific guidance.
It’s no secret that surgery can be stressful, but staying at the right recovery center can go a long way in making this journey a positive experience in the long run. The key is to plan your recovery in advance so you can focus on healing when the time comes.
A hip replacement is a positive step towards a happier and healthier life. While the prospect of surgery can be daunting, try to remember that the procedure is extremely common. You deserve to feel your best, so don’t hesitate to get in touch with your doctor if you feel like a hip replacement could be the right decision.
Isabella Koretz, Founder & CEO of Pearl Recovery Retreat and Ciel Spa, has been an entrepreneur and businesswoman for over a decade. Her experience in the healthcare industry is vast and she understands both the medical professional and patient side of the industry. While her professional endeavors are extensive, she is most proud of her role as a loving wife and a mother of two beautiful children.
References:
Images

According to the American Joint Replacement Registry, there are 860,000 total knee and hip replacements done in the United States per year. This number is projected to double in the next ten years. There are more knees than hips done per year and more females have these joint replacements than males.
 According to Mike Carberry of Advanced Medical Integration, “Regenerative medicine is one of the most talked about subject healthcare has ever known; and for good reason. It could hold the solution to the puzzle of America’s failed healthcare system.”
According to Mike Carberry of Advanced Medical Integration, “Regenerative medicine is one of the most talked about subject healthcare has ever known; and for good reason. It could hold the solution to the puzzle of America’s failed healthcare system.”
This is wonderful news for the personal training industry. Insurance is paying for less and less, costing more while the number of consumers seeking optimal health is increasing. A perfect storm in the making!
A personal training certificate, however, is not enough to appropriately deal with the typical client with total joint needs. Specialization in anatomy, joint physiology, biomechanics and therapeutic exercise are necessary in order to adequately and appropriately manage total joint conditions. These skills and techniques in conjunction with medical communication skills will give physicians confidence to send these patients to the appropriately skilled personal trainer. Spending time with a physical therapist and surgeon specializing in these areas will go a long way in establishing confidence, trust and credibility in handling the client with total joint conditions.
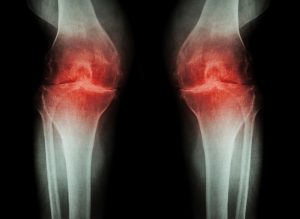
Most individuals with true joint pain have some level of osteoarthritis. Approximately 27 million Americans suffer from degenerative joint disease (also known as degenerative arthritis or osteoarthritis). Degenerative joint disease is the most common chronic condition of the joints and occurs most often in knees, hips, lower back and neck, small joints of the fingers, and the bases of the thumb and big toe.
Osteoarthritis is the most common form of arthritis that causes a breakdown of joint cartilage, and it affects mostly middle-aged and older adults.
Although there is no cure for osteoarthritis, the good news is that it can be helped, and quality of life maintained by implementing and maintaining some simple changes in daily life. Regardless of the intervention, from routine steroid injections to platelet rich plasma/stem cell treatments to total joint replacement, here are a few areas where the personal trainer can intervene with great success.
Exercise is key component of arthritis care, exercise strengthens the muscles, lessens joint pain and stiffness and improves overall health. Types of recommended exercises may include strengthening, aerobic activity (aquatic activity is wonderful), range of motion or stretching activities and balance exercises.
Protect the joints to ease pain and avoid further damage. Make sure to balance rest with activity as well as know when to stop. A good rule of thumb is to adjust down the frequency, intensity and duration by 50% of what a “normal” client can do or what the client thinks they can do. Remember these clients are typically deconditioned relative to strength and cardiovascular fitness. They will not handle the all-too-popular high-intensity interval training (HIIT). This population will succumb to overload and may be injured.
Pain control routinely treated with prescription or over-the-counter medications can be replaced or augmented by relaxation techniques (yoga, Tai Chi, meditation and massage) along with application of heat, cold and/or vibration.
If the client has had regenerative therapy or a total joint replacement, they will need a specific post-procedure plan to allow for healing/protection, early intervention and return to activity function. Hopefully, they had pre-intervention care inclusive of appropriate exercise, nutritional counseling and insight on what to expect with the procedure and post-procedure care. Appropriate nutrition for optimal health and healing along with hydration techniques and insights are a must during these sessions.
Typical post-procedure care is in three to four phases. Phase one is protect/rest, restore and control pain. During this phase the focus is on mediating pain, restoring range of motion, controlling swelling and protecting the joint. This is typically fourteen to twenty-one days in duration. Stitches or staples are usually removed at this time and scar management can commence around the twenty-first day.
Phase two is the restore and regenerate phase. The
wound is healing (healed), the joint and soft tissue healing continues, and remodeling of tissue has begun. This phase is typically three to six weeks in duration. Techniques to restore range of motion and other soft tissue techniques to facilitate healing according to tissue physiology and the client’s general health are initiated (conditions such as diabetes, obesity, cardiovascular disease and others will alter the healing and remediation phases). Techniques for ambulation, gait and balance are initiated along with appropriate cardiovascular conditioning.

Phase three typically commences when the client has gained full range of motion, has good balance and gait mechanics and is able to tolerate closed-chain activities for both upper and lower extremity movement patterns. This phase is the final phase and progresses to full functional activity and return to sport or recreational activities of choice (these activities may be placed into a fourth phase). During this phase it is incumbent upon the personal trainer to load appropriately and have working knowledge of the mechanics of the sport or recreational activity. There are some tremendous resources available for this purpose.
Complications to be aware of when working with these patients include but are not limited to infection, blood loss, dislocation, blood clots and fatigue. The personal trainer should also be in contact with the client’s physician and physical therapist if one has been engaged. These are medical conditions requiring communication and conservative care.
Most physicians like to know who is working with their patients and appreciate the communication for optimal outcomes. The insightful and knowledgeable personal trainer with the right training can be an invaluable member of the total joint care team. The future is bright!
This information is provided as an overview and in no way should be interpreted as a protocol for treatment or otherwise. Our goal is to inform the reader on opportunities in the profession and stimulate further investigation.
This article was featured in MedFit Professional Magazine.
Dr. Stephen A. Black is a sports medicine specialist, author and clinician. His doctoral degree is in sports medicine and he holds degrees in physical therapy, athletic training and certification through the National Strength and Conditioning Association. Dr. Black has over forty years’ experience in patient care and practice management. He lectures frequently on topics in sports medicine, works with professional, Olympic and youth athletes and holds several academic appointments. Visit his website, rockymountainhpc.com

Arthritis is the most common cause of disability in the world.3 Osteoarthritis, the most common form of arthritis, has led to a dramatic increase in the incidence of hip and knee replacements in recent years. The rate of total hip replacements has almost doubled between the years 2000-20101 and approximately 7.2 million Americans are now living with hip and/or knee replacements. 6 While these rates have nearly doubled in recent years, the number of younger individuals (ages 45-54) having these replacement surgeries is increasing.5
 The rapid and dramatic increase in individuals living with osteoarthritis and/or joint replacements has created a massive void between the number of people living with these issues and the number of qualified individuals to help them safely and effectively accomplish their functional goals. This void, however, has created an incredible opportunity for fitness professionals to align themselves with allied health professionals to become part of the solution. This article will discuss some recent changes in the thought process about how osteoarthritis develops, how fitness professionals are an important part of the solution, and why this is the most opportune time for fitness professionals to specialize and align themselves with health professionals.
The rapid and dramatic increase in individuals living with osteoarthritis and/or joint replacements has created a massive void between the number of people living with these issues and the number of qualified individuals to help them safely and effectively accomplish their functional goals. This void, however, has created an incredible opportunity for fitness professionals to align themselves with allied health professionals to become part of the solution. This article will discuss some recent changes in the thought process about how osteoarthritis develops, how fitness professionals are an important part of the solution, and why this is the most opportune time for fitness professionals to specialize and align themselves with health professionals.
While injury, overuse, age, obesity, genetics, and race have been given as possible causes, there has been a lack of solid evidence to explain why the incidence rate of osteoarthritis continues to skyrocket. 2,3,5 However, recently there have been suggestions that osteoarthritis is not as previously suggested, due only to old age or genetics. Dr. Ian Wallace, a postdoctoral researcher who has studied more than 2,000 skeletons, believes the recent dramatic increase in osteoarthritis isn’t an inevitable consequence of living longer. He believes it is more attributable to the modern decline of physical activity and is quoted as follows: “Dr. Wallace thinks the most obvious candidate to explain the increase in knee osteoarthritis is the modern decline in physical activity.” 8
Nevertheless, it is not just about people needing more quantity of activity; it’s also about the quality of the exercise.10,11 If exercise is performed without optimal joint alignment and control, the individual is at risk for developing degenerative joint changes.10,11 Therefore, it’s imperative that fitness professionals specializing in working with individuals that have osteoarthritis or joint replacements are able to properly assess for non-optimal and inefficient posture and movement habits and from these results, develop an appropriate exercise program. Additionally, fitness professions specializing in this niche must also be able to instruct proper exercise form and understand what exercises or activities are contraindicated with these populations. 10,11
A well-designed exercise program that includes flexibility, strength, and cardiovascular exercise is required to appropriately address the postural and movement habits that contributed to the development of osteoarthritis. Likewise, many individuals will have developed compensatory patterns as a result of joint pain or loss of mobility and subsequently developed non-optimal posture and movement habits that need to be addressed.
Several organizations including the Arthritis Foundation, Center for Disease Control, and American College of Sports Medicine have created guidelines for working with individuals that present with arthritis. General recommendations include improving joint mobility/flexibility, aerobic conditioning, resistance training, maintaining a healthy weight, and consulting with a medical doctor.2,3,13
Helping individuals develop a more optimal and efficient posture and movement strategy is one of the most effective strategies for safely working with individuals with osteoarthritis and joint replacements.9,10,11 An approach that includes using the most appropriate soft tissue release, mobilization, stretching, neuromuscular activation strategies, and appropriately progressing the individual through the fundamental movement patterns has been shown to improve joint mobility and strength in individuals with osteoarthritis as well as joint replacements. 9,10,11 Additional strategies that have been shown to be helpful in improving strength and mobility and managing the symptoms of osteoarthritis include three-dimensional breathing7,9,10,11, proper nutrition featuring a whole-foods, plant-based diet4, and meditation.14

The great news is that there is a growing need for qualified fitness professionals to work with the increasing numbers of individuals that have osteoarthritis and/or joint replacements. However, this requires that the fitness professional have both the right education and the appropriate skillset as many of these individuals will require a thorough approach to address their specific needs and to provide them with the best functional outcomes. Organizations such as the MedFit Education Foundation are helping to create the education necessary for health and fitness professionals to develop specializations in working with special populations including the older adult populations experiencing osteoarthritis and joint replacements. Additionally, through their educational platforms and live course work, they provide fitness professionals with strategies for aligning and working with allied health professionals.
For many individuals experiencing pain or loss of function secondary to osteoarthritic changes, seamless integration between medical procedures, rehabilitation, and functional fitness is becoming a viable and necessary alternative to narcotics and surgery. Hence, the birth of the medical fitness space where fitness professionals work either in collaboration with or in the actual physical location of medical doctors, physical therapists, chiropractic physicians, and massage therapists. Clinics such as Rejuv Medical have provided a model for how to improve patient outcomes by combining the benefits of regenerative medicine procedures (Plasma Rich Protein and Stem Cell Therapy), physical therapy, and personal/group training.
Specialization in working with individuals that have osteoarthritis and/or joint replacements and working in the medical fitness space is the future. The fitness professional that acquires the appropriate education and develops a working relationship with allied health professionals will be able to attract more individuals that need, want, and will pay for their expertise. By providing a more integrated and effective approach to helping individuals accomplish their health and fitness goals, these fitness professionals will continue to thrive in the coming years.
This article was featured in MedFit Professional Magazine.
Dr. Evan Osar is an internationally recognized speaker, author, and expert on assessment, corrective exercise, and functional movement. Dr. Osar is committed to educating and empowering fitness professionals while helping them develop relationships with allied health professionals. He is author of the Corrective Exercise Solutions to Common Hip and Shoulder Dysfunction and has developed the industry’s most complete training certification, the Integrative Movement Specialist™. With his wife Jenice Mattek, he created the on-line educational resource www.IIHFE.com.
References: