Muscles: Don’t Take Them for Granted
Do you ever have pain in your muscles and joints when you move around? I did… and still sometimes do! I started my career as a Personal Trainer 20 years ago at Oak Hill Country Club in Rochester, New York . . .
Lost your password? Please enter your email address. You will receive a link to create a new password.

Do you ever have pain in your muscles and joints when you move around? I did… and still sometimes do! I started my career as a Personal Trainer 20 years ago at Oak Hill Country Club in Rochester, New York . . .

Time is one of life’s most valuable commodities. Consequently, between school, work and every day demands in today’s hectic world, family time is becoming more of a fond memory of days gone by. Additionally, television, computers, cell phones, and other technology are taking the place of family activities and interactions.
The decline in positive family interactions at home, and the increase in leading a more sedentary lifestyle, are two of the greatest threats to our children’s health and wellness.
According to the National Alliance on Mental Illness (NAMI), “family has a big influence on how we perceive exercise and mental health. Exercising as a family not only gets the entire family moving to reap the benefits of exercise but also models healthy beliefs about physical activity and improves family relationships”. And with childhood obesity becoming a nationwide epidemic, getting kids moving and active is extremely vital.

As parents, we want only the best for our children’s future. Making time for simple and fun family activities can have a profound impact on the mental and physical well-being of every single family member, both young and old!
Here are some fun, budget-friendly ways to bring your loved ones closer together and get a little exercise at the same time!
1. PLAY: Avoid television for family entertainment. Go to the park and play, have a family sports night (soccer, basketball, etc.), play Frisbee, hop scotch, or get a mini trampoline.
2. PETS: If you have a dog or other pet, actively play with them as a family and even take them on a family walk.
3. SWIM: Go to the beach, lake, or public pool. Swimming is fun and lively, and your family won’t even realize they are getting exercise.
4. WALK: Walk to the store, walk to school, etc. Get pedometers for the whole family and see who can rack up the most steps. Certain ones even log your steps online or through apps, so you can expand the contest to your friends and other families.
5. ADVENTURE: Every weekend, try a new activity your family hasn’t done yet. Hiking, bowling, canoeing, ice-skating, etc., all are active exercises disguised as fun. Let each member of the family have their turn to pick the next activity, so they stay involved.
6. GYM: Join a gym that offers family discounts, and work out together. If you can afford a personal trainer, they can organize a routine for each family member.
7. WILDLIFE: Visit a zoo, wildlife preserve, or an aquarium where you’ll be walking most of the day.
8. GIFTS: When birthdays and holidays come around, give gifts that encourage fitness. Jump ropes, Frisbees, running shoes, balls, active toys, etc., can all inspire your family to get up and get moving.
9. STAIRS: Encourage your family to take the stairs, instead of the elevator, whenever possible. If they object, make a creative game out of it.

10. REWARD: Exercise can be a reward. Offer to play catch with them or play a game of kickball or capture the flag as a break from homework or chores.
11. FRIENDS: Invite your child’s friend along for any of these activities. Kids have more fun with their friends, and are more likely to want to do it again.
12. FUN: Make things fun! Build an obstacle course with your family and have everyone participate. Have hula hoop contests or play active games like hot potato, Simon Says, and Duck, Duck, Goose. The internet is a great source for finding new games to play.
13. CHORES: Household chores done as a family can be great exercise (cutting grass, cleaning, etc.). You can also make chores fun by adding a “challenge” element. Kids love challenges. “I challenge you to put away all your toys in 1 minute.” You can have a fun family reward at the end like fruit popsicles.
14. DANCE: Dancing is a great form of exercise and is a lot of fun. You can have the kids each pick their favorite song and even have themed dance nights where you dress up in funny outfits.
Kendra K is an award-winning music artist with a passion for educating and entertaining children. She is a seasoned singer, songwriter, producer, pianist and violinist with a Bachelor of Science degree in Education from the University of Arizona. Kendra has worked as a physical education teacher and is also certified as a national health and fitness consultant. When Kendra is not busy writing songs and recording albums, she enjoys donating her time and talents as a children’s health advocate. Her biggest joy in life is spending time with her husband and their young son at their beach side home in the Los Angeles area.
Visit her website, kendrakmusic.com and her new children’s music CD is available through Amazon or CD baby
References:
https://www.nami.org/Blogs/NAMI-Blog/May-2016/Exercise-for-Mental-Health-8-Keys-to-Get-and-Stay
https://www.hhs.gov/fitness/resource-center/facts-and-statistics/index.html

“[Whole Person Integrative Eating] provides a fresh perspective on our epidemic of overeating, overweight, and obesity…that…could signal a paradigm shift in the field of nutrition.” . . .

You have back pain, and you’re determined to beat it. You’ve been to your doctor and received pain and anti-inflammatory meds. You’ve been to massage therapy to relax the tight muscles….

If there’s anything certain about MS, it’s the uncertainty of the disease. Energy, strength and mobility can fluctuate over the years – especially if you’re living with Relapsing Remitting MS.
 So it’s important, when considering an exercise plan, to have options that you can scale and honor your body.
So it’s important, when considering an exercise plan, to have options that you can scale and honor your body.
Personally, I’ve always loved exercising. So my ability to maintain a consistent schedule is something I treasure. I start my mornings either at CrossFit or going for a run.
This is what works for me now.
Shortly before I was diagnosed my “workouts” looked drastically different.
The fatigue was so extreme, the most movement I could do was a child’s pose on the floor next to be bed. Slowly I worked my way to walking around the neighborhood and eventually as I went into remission I developed the stamina to strength train.
The most important thing to know when developing an MS-friendly exercise plan is to always honor what your body can do in the given moment.
Sometimes that means giving yourself a pep-talk to take a stroll around the block even though you’re feeling a little down. Other times, you may need to scale back your efforts as anyone with MS knows, the fatigue is not something you “push through.”
Only you can be the true judge in striking that right balance – and it will likely be a fluid process. But keep in mind, even small efforts with diet and lifestyle can add up to create a healing environment in your body.
Need some ideas on where to start? Check out these New Exercises and Activities to Try if You Have MS.
This post originally appeared on www.alenebrennan.com. Reprinted with permission.
Alene Brennan has been featured in USA Today, Philadelphia Inquirer, Huffington Post and Mind Body Green. Alene overcame debilitating migraine headaches through diet and lifestyle and is now once again using a “Less Pharm, More Table” approach is managing her diagnosis of Multiple Sclerosis. Alene holds four certifications: Nutrition Coach, Yoga Instructor, Personal Trainer and Natural Food Chef. She also completed specialized training in nutrition for autoimmune disease specifically the Wahls Protocol and the Autoimmune Protocol. Since receiving her MS diagnosis and seeing first-hand the power of using diet and lifestyle to create a healing environment in the body, she dedicated her virtual nutrition coaching practice to helping people with MS and autoimmune dieseases take back control of their health. Visit her website, alenebrennan.com.

 Many athletes train in the early morning. Rowers commonly meet at 5:30 a.m. Hockey players might get rink-time at 5:00 a.m.. Athletes who need to be at work at 7:00 often train at 4:30 a.m. Many of these athletes report eating nothing before their training session. My stomach isn’t awake. … It’s too early to even think about food. … I get reflux if I eat. Others report they have better workouts when they eat something simple. The question arises: What’s the best way to fuel for early morning workouts?
Many athletes train in the early morning. Rowers commonly meet at 5:30 a.m. Hockey players might get rink-time at 5:00 a.m.. Athletes who need to be at work at 7:00 often train at 4:30 a.m. Many of these athletes report eating nothing before their training session. My stomach isn’t awake. … It’s too early to even think about food. … I get reflux if I eat. Others report they have better workouts when they eat something simple. The question arises: What’s the best way to fuel for early morning workouts?
Before answering that question, let’s first address the physiological goals for fueling before morning workouts.
1) To change the stress-hormone profile. Cortisol (a stress hormone) is high in the early morning. This puts your body in muscle-breakdown mode. Eating carbs + protein can switch to muscle-building mode.
2) To provide energy and prevent low blood glucose with the consequences of feeling light-headed, dizzy, and needlessly fatigued.
3) To be adequately hydrated. Dehydration slows you down.
If you are making the effort to get up early to train, you might as well get the most out of your workout! In a fueling study, athletes had dinner the night before and then a 60-minute exercise test the next morning. They performed 6% better in the 10-minute sprint to the finish when they had some fuel (carb) compared to having had nothing; 6% better when they had adequate water (compared to minimal water), and 12% better when they had both fuel + water (a sport drink). (1) Twelve percent better means running an 8-minute mile in about 7 minutes. Powerful, eh?
Your body can digest pre-exercise food and use it to energize your exercise as long as you are exercising at a pace that you can maintain for more than 30 minutes. (If you do stop-and-start exercise, you can still digest the food, but at a slower rate.) In another fueling study, athletes ate dinner and than nothing for the next 12 hours. Those who ate 180 calories (sugar) just five minutes before an hour-long exercise test performed 10% better in the last 15 minute sprint compared to when they ate nothing (2). Grab that granola bar or swig of juice!
If you are tempted to skip pre-exercise food so you can lose weight by burning more fat, think again. Yes, pre-exercise food will contribute to burning less fat at the moment, but that is irrelevant. The issue is not whether you have burned fat during exercise but if you have created a calorie deficit by the end of the day. Eating excess calories after a fat-burning workout gets you nowhere.
All of this means consuming some food and fluid on your way to the gym, spin class, or boot camp will enhance your workout—assuming you have trained your gut to tolerate the food and fluids. If you are worried about intestinal distress, start small (a few crackers) and work up to a handful of crackers, and then add, let’s say, a latte. For workouts longer than 60 minutes, the recommended intake is about 200 to 400 calories within the hour before you train. That recommendation obviously varies according to body size, exercise intensity and duration, and personal tolerance to food.
If you have been exercising on empty, you will likely discover you can exercise harder, feel better, and get more enjoyment from your workouts. Research subjects who ate 400 pre-exercise calories were able to exercise for 136 minutes until they were exhausted, as compared to only 109 minutes with no breakfast (3). Big difference! After learning this, one of my clients reported he was done with skipping pre-exercise fuel in the name of intermittent fasting. “Not eating is slowing me down and taking the fun out of my workout.”
 Early morning options
Early morning optionsHere are some options for fueling your early morning workouts so you are adequately hydrated and fueled.
Eat a quick and easy snack with about 200 to 400 calories (depending on your body size and workout intensity). Some popular options include: English muffin, toast, bagel or banana (with peanut butter); oatmeal, a smoothie, Fig Newtons, or granola bar. Coffee is OK; it’s a functional fluid that boosts performance and yes, helps with hydration.
Wake up 4 hours before important training sessions/events, eat a simple breakfast (bread + peanut butter), then go back to bed. This is a common practice among elite athletes. As one marathoner explained, “I don’t want to have food in my stomach when I’m racing. If a race starts at 8:00 a.m., I’ll get up at 4:00, eat a bagel with peanut butter and a banana, and then go back to bed. At 6:00, I’ll get up, have some coffee (to help me take a dump and wake me up), and then get to the race start. Because I never really sleep well the night before an event, getting up at 4:00 isn’t terribly disruptive.” In comparison, a rower reported she used to wake up two hours before practice to eat. She became too sleep-deprived and decided she needed sleep more than food. She started eating a bigger bedtime snack.
Eat your breakfast the night before via a bedtime snack, such as a bowl of cereal, or yogurt with granola. If you have dinner at 6:00, you’ll be ready for a bedtime snack by 9:00. Choose quality calories; this is your breakfast that you are eating the night before. Limit the cookies and ice cream!
Fuel during your workout.If your stomach isn’t awake when you first get up, it may be receptive to fuel when you are 30 minutes into your bike ride, run, or row. Be sure you have some fuel with you: sport drink, dried pineapple, gels, chomps, gummy bears—whatever is easy to carry and simple to digest. You want to target about 30 to 60 grams carb (120 to 240 calories) if the workout lasts 1 to 2.5 hours, and 60 to 90 g carb (240 to 360 cal) if the workout is longer than that..
If you are highly competitive and has mastered the sports nutrition basics (eat a diet with 90% quality foods; fuel evenly during the day; have no disordered eating behaviors), you might try training low (with depleted muscle glycogen and/or low blood glucose) once a week or so. To do this, eat primarily protein for dinner after a late-afternoon workout. The next morning, train without having eaten carbs. Exercising depleted like this is not fun, but it stimulates cellular changes that can be performance enhancing if you need to get to the next level (4). Novice and recreational athletes, however, first need to work on the basic ways to improve performance—by surrounding their workouts with food, and fueling wisely the rest of the day.
Nancy Clark, MS, RD counsels both casual and competitive athletes at her office in Newton, MA (617-795-1875). Her best selling Sports Nutrition Guidebook and food guides for marathoners, cyclists and soccer players offer additional inform-ation. They are available at NancyClarkRD.com. For her online workshop, visit NutritionSportsExerciseCEUs.com.
References

Parkinson’s Disease is a brain disorder that causes individuals to have difficulty with balance, coordination and walking. They can also become shaky or stiff and some people even develop tremors. It is a common disease that can….

I hope to give you some insights to both how the human body works as well as why medically-based fitness is not only valid, but absolutely necessary to reverse, assist, or prevent various chronic and acute disease conditions. Wow, that is a “mouthful” to say the least. I feel so strongly about this perspective that I hope to create the Adaptive Health Model as a major “brand” of fitness. My company (Principle-Centered Health) for the past couple of decades has always had a systems-based approach to health and fitness. This approach ties a lot of different facts into a common theme, usually called a theory in science. Even my dissertation looked at how people adapted to the physical, mental and social issues in their lives using exercise, self-efficacy, and social support, respectively, and levels of strain and burnout. How humans adapt to the stresses put on them is very specific and can go in good or bad directions.

Like most theories, paradigms or what people consider “original thought”, this “adaptive” paradigm builds on the “regenerative medicine” framework, and some disease models; thus, is not original at all. What may be new, or unique about the adaptive perspective is taking the old phrase from physicist Isaac Newton and his third law of motion, “for every action there is an equal and opposite reaction.” The body will respond to stresses by reacting in a “defensive” manner. If we break something down, the body builds it up (opposite reaction). If we are too low or too high in some function, the body will try to correct this. This negative feedback loop controls most systems in our bodies. I have often described our bodies as fragile but resilient. It is our fragility that signals the resilience to kick into gear!
Luckily for us, fitness is based on this exact principle. If we do endurance training, we are going into a lower oxygen state and there are many mechanisms or functions that kick in (sympathetic nervous system) when we push or stress our bodies. The body is responding to what is known as an “acute insult” by increasing the ability to transport and use oxygen, so that this “insult” doesn’t hurt us next time. The same “specificity of training principle” occurs with resistance training. We breakdown muscle and the body builds it back stronger to tolerate that “insult” the next time. When multiple acute exercise stresses are added up, the body changes and we call this “training”.
If stresses are really high, either too intense, too long, or too often, the body gets injured due to this overload, or it needs a lot more time to heal back up. This is why overload needs to be done gradually and progressively. Even our brains use this idea as a guiding principle. We push our mental capacities to learn more, but if we stress it too much, it will repress memories or shut down (burnout).
This same principle applies when we give our body bad things, or a lack of good things, it adapts with a dysfunctional state or disease state. Chronic inflammatory diseases, diabetes, metabolic syndrome, coronary artery disease, emphysema and heart disease are just a few of the examples of how the “garbage in and garbage out”, or “use it or lose it” works. If we sit and work at the computer too much we develop dysfunctional postures and upper cross syndrome may develop. If we do not constantly stress some system, it reverses the training changes, and goes into the “default” state, which is untrained and unable to respond to daily stresses. We simply need to obey our bodily blueprints, we need to constantly use our bodies to maintain function, and overload it to improve function. We need to have the right nutrients in place to allow this to happen, and then basically – get out of the way!
The perspective being proposed in this article shares much with the more holistic medical practices. The human body is really good at healing itself when is it given the right factors to do so, and when we “get out of the way” for it to do so. I know many people who strongly believe in using alkaline water to “cure their ills”. They believe that the body does not know how to regulate itself with its own pH. Most of these same people don’t know what pH even stands for! They don’t know that it is actually the inverse log of the hydrogen ion concentration relative to the hydroxide ions, and that the respiratory system and renal system will go into action as soon as blood pH goes 0.05 pH units high or low!
In other words, these people believe their own bodies are naïve or incapable of curing itself, and like a young child or baby, their body needs constant care and guidance. Most people are so stressed about “taking care” of their bodies that they are doing more harm than good via the stress hormones, especially cortisol being constantly secreted and their adrenal gland is getting fatigued. In reality, the body is really good at healing itself, when we keep it strong and in good operating condition (via exercise and movement) and when we give it the right components to do the healing (via nutrition), and we get out of the way of the immune system (by managing our daily stress levels).
The mind works very much like a muscle. It must be trained and kept strong and when injured it will react in dysfunctional ways, and fight to protect itself. I recently heard an expert in human behavior change speak on how to keep a resolution. He said, we can’t keep a resolution without changing the underlying behaviors which caused the bad habit or lack of a good habit in the first place. By changing the way we think, we change the way we act, and changing our actions will change the way we think!
The quote often stated by Thomas Edison in 1903, which was to give rise to the HMO concept, “The doctor of the future will give no medicine, but will interest his patient in the care of the human frame, in diet and in the cause and prevention of disease.” Medical doctors (M.D.s) upon completing medical school and prior to practicing take the Hippocratic Oath, which is to do no harm. Even back in Ancient Rome, Hippocrates understood the importance of individualized medicine and the power to “get out of the way” (#5) and give the body what it needs to take care of itself. He had five rules that are still relevant in today’s medical practices.
A philosophy of practice using these practices is integrative medicine. A brand of medicine created or at least popularized by Andrew Weil. The University of Arizona has this “brand” of medical school. Again, the academic requirements are similar to the M.D. and D.O. but expands its scope to other areas. From the website, Integrative Medicine (IM) is defined as a “healing-oriented medicine that takes account of the whole person, including all aspects of lifestyle. It emphasizes the therapeutic relationship between practitioner and patient, is informed by evidence, and makes use of all appropriate therapies. many different ways in the patient.
A new type of medicine is emerging from this functional perspective which is called personalized medicine. Again, the two are basically two sides of the same coin.
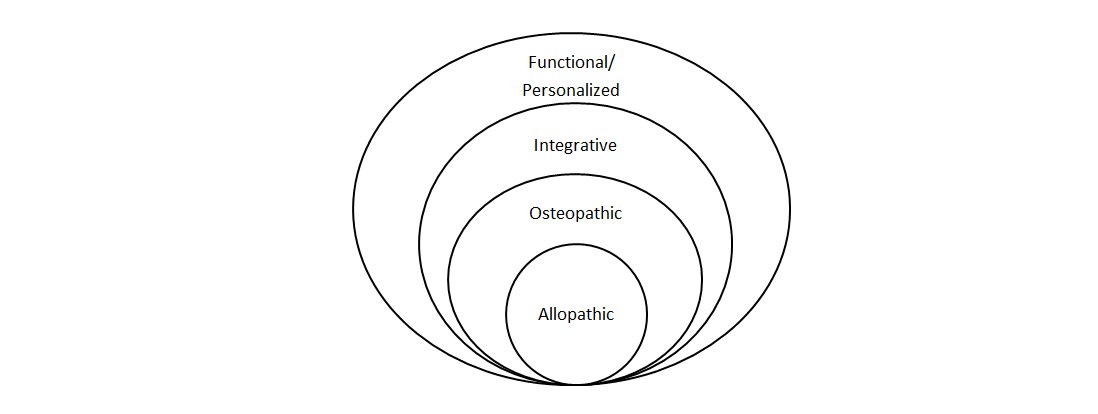
Figure 1: A diagram above showing the greater scope of each medical perspective- Integrative and Functional medicines are close in their holistic perspectives, with differing points of emphasis
Sometimes disease hits simply because we were genetically predisposed to get it. However, very often if our system is strong and in good operating condition, we resist it from every occurring or overcome it quite quickly. Cancer is a prime example of this. We all have cancers in our bodies all the time. It is the strong immune system that fights it off. This is amongst the reasons that many, many chronic diseases hit us when we are old. The various system have lost their capacity to fight the dysfunction off, or recover from its destruction. Soon cell death (necrosis or apoptosis) or neoplastic (cancer) growth kicks in.

Many, many chronic conditions that the MedFit Network and MedFit Classroom address are helped by exercise and diet because the ability of body to adapt and regenerate itself is enhanced. Most systems in our body fall under the “use it or lose it” scenario. High sugar, alcohol, smoking, and lack of movement are culprits in our health. Our body is not designed for an overload of these factors and across time, many different symptoms will develop because our body can no longer compensate or regenerate.
It is important for the medical fitness professional to understand the power of exercise and nutrition, and the proper application of these tools given the client’s or patient’s current condition. The field of physical therapy developed because many musculoskeletal conditions are helped by movement therapy or exercise. Many chiropractors believe that proper spinal alignment delivers proper neural signals throughout the body, which allows the body to optimize its regenerative capacity. Thus, an expert in medical uses of exercise to combat disease is critical to a healthcare team.
Dr. Mark Kelly Ph.D., CSCS, FAS, CPT has been actively involved in the fitness industry spanning 30 years as a teacher of exercise physiology at academic institutions such as California State University, Fullerton, Louisiana State University, Health Science Center, Tulane University and Biola. He was an exercise physiologist for the American Council on Exercise, a corporate wellness director, boot camp company owner and master fitness trainer.
References
Center for Integrative Medicine, Univ. of Arizona (n.d.). What is IM/IH? Retrieved from: https://integrativemedicine.arizona.edu/about/definition.html
Science Daily (n.d.). Personalized medicine. Retrieved from: https://www.sciencedaily.com/terms/personalized_medicine.htm
Good Reads (n.d.). Retreived from: https://www.goodreads.com/quotes/13639-the-doctor-of-the-future-will-give-no-medication-but
Kalish, N. (2018). Hippocrates’ Diet and Health Rules Everyone Should Follow. Reader’s Digest. Retrieved from: https://www.rd.com/health/wellness/hippocrates-diet/

What drives you? Motivation is one of the most common objections I hear around why people don’t achieve their fitness and fat loss goals. As a result, there are 4 types of motivation . . .